Stress and depression can bring on irritable bowel syndrome
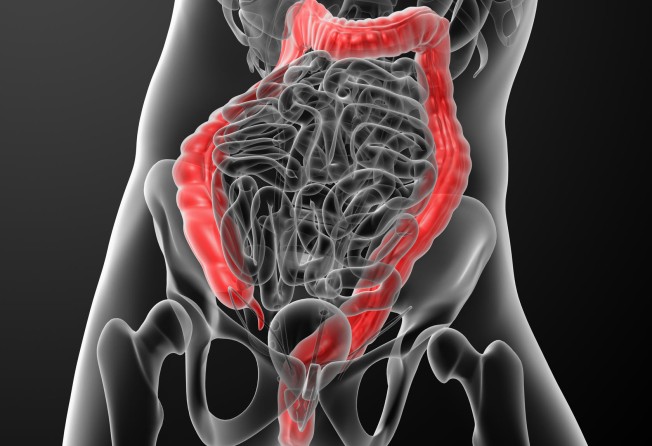
Irritable bowel syndrome (IBS) is an illness many have heard about, but is still poorly understood. The chronic, often disabling gastrointestinal condition leads to crampy pain, gassiness, bloating and changes in bowel habits. It can have detrimental effects on sufferers' quality of life.
In two studies based in Hong Kong, the prevalence of IBS was found to vary between 3.7 per cent and 6.6 per cent, according to a review published in Alimentary Pharmacology & Therapeutics in 2005 by Dr Kang Jin-yong of the department of gastroenterology at St George's Hospital in London. Studies from North America reported a prevalence of between 12 per cent and 25 per cent.
Dr Edwin Lam Chi-wan and Dr Cheung Ting-kin, both gastroenterologists in Hong Kong, say about half of the patients they consult have IBS. Most patients consulting specialists are worried about bowel cancer.
The diagnosis is made by recognising symptoms which have occurred for three months: lower abdominal pain; bloating; relief of pain with defecation; associated constipation or diarrhoea, or both.
Furthermore, IBS can only be diagnosed after other serious conditions have been ruled out. For example, if a patient has these symptoms but also has unintentional weight loss, investigation is needed to eliminate bowel cancer.
IBS is particularly common at times of stress or depression. This is because during prolonged periods of heightened emotional states, uncontrolled messages may be fired from the brain through the nervous system to the bowel, which may lead to uncoordinated contraction and relaxation of the muscle wall.
Studies have also shown that stress alters brain-gut interactions and induces the intestinal inflammation that leads to chronic belly pain, loss of appetite and diarrhoea.
Some individuals may have more sensitive visceral perception, which can give the sensation of abdominal pain.
There have been other hypotheses on the cause of IBS, such as abnormal bacteria growth or food intolerances.
Due to the wide range of symptoms that can occur, I suspect there is no single cause underlying this condition but rather a combination of them. Because of the unknown origin of IBS, there is no cure. Remedies can only alleviate symptoms, and are effective in some patients but not in others.
In January last year, scientists from 19 European countries joined forces to form an interdisciplinary network for investigating the causes of IBS in the hope of improving its diagnosis and treatment.
Named Genieur (Genes in irritable bowel syndrome Europe), the network aims to identify genes and DNA variants that may contribute to increase one's susceptibility to develop symptoms.
Until research reveals more clues to the condition, IBS sufferers can find relief by reviewing and managing their lifestyle and diet. In particular, patients may benefit from more regular exercise, as well as a reduced intake of caffeine, alcohol and nicotine, according to Dr Oliver Grundmann of the University of Florida in his paper published in 2010 in the Journal of Gastroenterology & Hepatology.
Researchers at Monash University in Australia have developed a new dietary management approach - the low Fodmap diet - to control symptoms associated with IBS. Fodmaps - or fermentable oligo-saccharides, disaccharides, monosaccharides and polyols - are a group of carbohydrates identified by the researchers that can be poorly absorbed in the small intestine. Badly absorbed carbohydrates are fermented by gut bacteria to produce gas.
Fodmaps are found in a wide range of foods, including vegetables (asparagus, onion, legumes/pulses, beetroot, celery, sweet corn); fruits (apple, pear, mango, watermelon, peach); dairy (cow's milk, yogurt, soft cheese, ice cream); wheat-containing breads, cereals, pasta and biscuits; and nuts and seeds (cashews, pistachios).
Some patients may find dietitian supervision helpful to find the right nutritional balance when excluding these foodstuffs.
Lam notes that many of his patients are lactose intolerant and has told them to stop drinking milk and to use enzyme supplements that break down lactose.
Those worried about not getting enough calcium might want to take vitamin D tablets. Evidence for avoiding gluten (bread and pasta) has not been particularly strong in IBS.
Tests for food allergies are available, but are not helpful in distinguishing what types of food exacerbate IBS symptoms. It is often better for the patient to keep a food diary by excluding certain foods for at least two weeks to determine whether symptoms improve.
Probiotics may reduce stress-induced intestinal flare-ups, says a University of Michigan study published in the journal Gastroenterology last year.
Probiotics are live bacteria that help grow the gut-dwelling "good" bacteria that keep pathogens in check, aid digestion and nutrient absorption and contribute to immune function.
In the study, pre-treatment with probiotic therapy reduced inflammation in mice with stress-induced small bowel inflammation.
When dietary advice has not helped, drug intervention may be required. For example, laxatives are beneficial in constipation. Lam uses Metamucil to treat patients with constipation as well as diarrhoea. The psyllium fibre supplement enhances bowel movements.
Cheung uses probiotics initially and, if ineffective, prescribes an antibiotic called Rifaximin to treat patients with bloating due to bacterial overgrowth. It has also been shown to work in IBS with diarrhoea.
Due to the association between IBS and mood, both Lam and Cheung have prescribed antidepressants to depressed patients with IBS with some success in pain control.
It can take time for these treatments to work, so patients may also benefit from attending psychological counselling.
As for complementary therapies, the jury is still out. Peppermint oil has also been used in conventional medicine to treat abdominal discomfort due to its effects on the smooth muscle wall of the bowel.
Acupuncture is no more effective than a placebo (using sham acupuncture where the needles are not inserted properly) in relieving IBS, according to a 2012 report which reviewed 17 studies.
Patients treated with traditional Chinese medicine showed no significant improvement in symptoms, according to a study led by Dr Leung Wai-keung of Chinese University published in The American Journal of Gastroenterology in 2006.
Dr Ray Ng is a member of the Royal College of General Practitioners (UK). He has a practice in Central. [email protected]