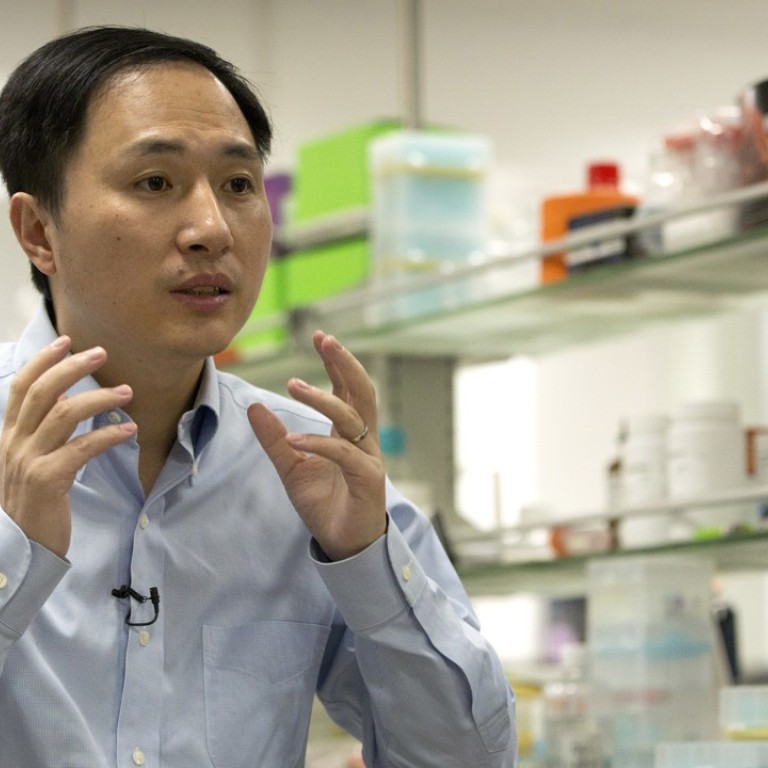
Gene editing won’t help the fight against HIV, understanding one’s risk and prevention options will
- Andrew Chidgey says HIV positive men and women can already have HIV negative babies through the use of medication and some well-recognised precautions
- This negates the need for gene editing to prevent transmission of HIV and raises ethical questions about a Chinese scientist’s recently announced research
My organisation is in daily contact with the public, answering questions about HIV, providing testing and supporting people living with HIV. When we understood more about the details of the research, we became deeply concerned that this could be damaging scientific research organised under unethical conditions.
The research was conducted with couples in which the man was HIV positive. The scientist changed the genetic material of some of participants’ unborn children to make them resistant to HIV. Two babies have been born, with more possibly on the way.
From a scientific point of view, one can marvel at the fact that it has become possible to do things as complex as changing the DNA of unborn children. However, great care is needed to ensure that scientific research is useful and safe, with sound ethics so that people are not mistreated during the process.
In my opinion, this project is of little benefit in the fight to stop new HIV infections. The risk of being infected by HIV can come through infection before birth or, more likely, later in life through sexual exposure. There are plenty of ways to stop this happening without the need for playing with genetics, where the risks and outcomes are unknown.
HIV positive men and women can now have HIV negative babies through the use of HIV medication and some well-recognised precautions. People living with HIV who hear about this research may think that they need to have their baby gene edited to prevent the baby from getting HIV. That isn’t true.
If a man is HIV positive but on HIV treatment with an undetectable viral load, he will not transmit HIV to the unborn child, or the mother, through his sperm. If, on the other hand, the mother is HIV positive, she can prevent transmission of HIV to her unborn child through being on HIV treatment, by having a caesarean delivery and not breastfeeding the baby.
So one can ask: what is the real value of introducing a technique where the risk of damage to a child is unknown and when there are safe, proven interventions that will stop the virus infecting the child?

The bigger ethical problem is the treatment of the parents and children in this research project
HIV cannot be transmitted through everyday physical contact with people who have HIV, such as by shaking hands or kissing, through toilet seats, mosquito bites or swimming pools. In fact, HIV treatment has now become so powerful that if someone with HIV has been taking a treatment for six months and has reached what is called an undetectable viral load, research shows they cannot pass the virus onto anyone else through sex. This is being described as “undetectable is untransmittable”.
I would argue that it is unethical to waste scientific resources on unneeded research and also to communicate the findings of research that isn’t responding to a useful scientific question. However, the bigger ethical problem is the treatment of the parents and children in this research project.
I want to know if the parents in this case were informed that with commonly available medical treatment their children would not be infected with HIV, without the need for gene editing where there is unknown risk to the children’s future health. Even if the parents did consent, is it acceptable to risk the health of the children when there are commonly available proven methods?
The international research community has been looking at the rules for conducting gene editing in scientific research. I would strongly urge them to have oversight and scrutiny of this research and to look at how to prevent inappropriate use of scientific research in the future. Without action, there is a risk of serious consequences
This World Aids Day, we are telling Hong Kong that we can stop HIV. People need to understand their own risk of HIV and decide what the correct prevention options are for them and those they care about.
Andrew Chidgey is chief executive of the Hong Kong Charity, Aids Concern

