Hong Kong’s management of the coronavirus epidemic is an evolving science, even after the lessons of Sars
- To be prepared for an outbreak is important but that provides only a framework. Any plan needs to be constantly informed by the emerging science in an epidemic, and complemented by real-time surveillance to gather effective intelligence in a fast-changing situation
On March 10, 2003, the severe acute respiratory syndrome unceremoniously announced its foothold in Hong Kong in an outbreak of the infection at the Prince of Wales Hospital, eventually infecting 239 health care professionals, medical students, patients and visitors.
It exposed Hong Kong’s vulnerability to new and emerging infectious diseases, in its geopolitical position and as an open economy with free flows of people, goods and services across its borders. Also evident were our public health inadequacies in surveillance for early detection and in rapid responses to threats.
Even the most robust preparedness plans, however regularly updated, can only provide a framework when there is insufficient knowledge and understanding of the nature of the agent and the range of its effects on the host. The application of strategies and measures to control the outbreak has to be assessed in real time as science unravels the mystery.
Is history repeating itself in Hong Kong’s battle with coronavirus?
The integration of data collected from both sources of surveillance should be synthesised and analysed for intelligence on dissemination risks. Early detection of infection enables a correspondingly rapid response, allowing for timely and effective contact tracing and surveillance of close contacts that are critical for containment.
Clinical management of infected patients and the health services’ infection control procedures and practices are key components of epidemic prevention and control.
World Health Organisation guidelines now recommend that close contact is defined as having been within a metre of an infected person during the symptomatic period, including four days before the onset of symptoms. Policies on medical surveillance and contact quarantine need to be readjusted.
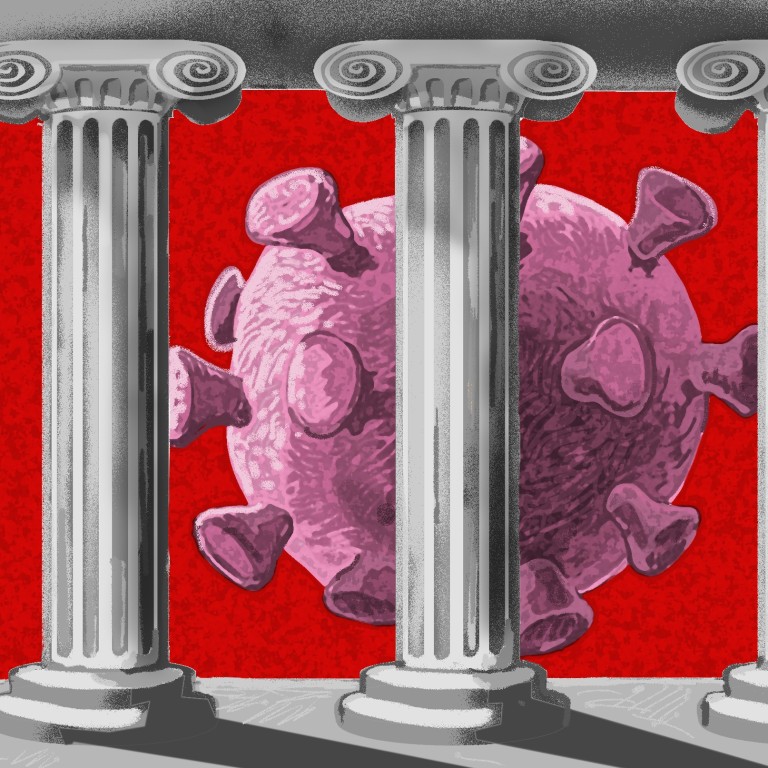
An effective and rapid response to the epidemic should be built on three pillars. One, leadership from the government. Two, partnership with public health academics to apply methods to facilitate the discovery of the interventions needed. And three, the community’s participation in control and prevention measures, and engagement in prevention and mitigating behaviours.
Risk communication is a crucial intervention in controlling an epidemic, and is a science in itself. It is prefaced on a deep understanding of the anxieties, perceptions and fears of the public elicited from ongoing research during the epidemic, so as to design content, format and modes of communication to persuade the community to adopt behavioural and social interventions to minimise the spread of infection.
This two-way communication should ideally be a real-time exchange of information, advice and opinions between public health authorities and the community.
Political judgment and critical assessment informed by current scientific knowledge and epidemic intelligence are crucial in the decision to stagger the easing of the restrictions to prevent a resurgence of infections.
Should a pandemic arise, sectors of the community would need to work with the government and offer constructive criticism; recriminations are unhelpful and may be counterproductive.
When the science is tentative, pronouncement and predictions need to be made with reticence and supported by epidemic intelligence. Otherwise, they are likely to be unhelpful at best, and detrimental to the efforts of containment at worst.
Yeoh Eng-kiong, a former health secretary of Hong Kong, is director of the JC School of Public Health and Primary Care, and head of the Division of Health System, Policy and Management, Faculty of Medicine at the Chinese University of Hong Kong

