
The latest on HIV prevention: five ways to curb spread of virus outlined by scientists at Paris conference
With HIV prevention ‘absolutely critical’ given there is still no cure, researchers from around the world present their findings on the benefits of circumcision, having less sex, antiretroviral therapy and more
A far cry from the 1990s “ABC” campaign promoting abstinence and monogamy as HIV protection, scientists reported this week on new approaches allowing people to have all the safe sex they want.
Moving away from the message to “Abstain, Be faithful, use Condoms”, modern prevention strategies include drug-doused vaginal rings, male circumcision, and taking antiretroviral therapy (ART) medication, experts said at a conference on HIV science in Paris.
Thirty-five years of research has yet to yield a cure or vaccine for the virus, which has infected more than 76 million people since the early 1980s, and killed 35 million.
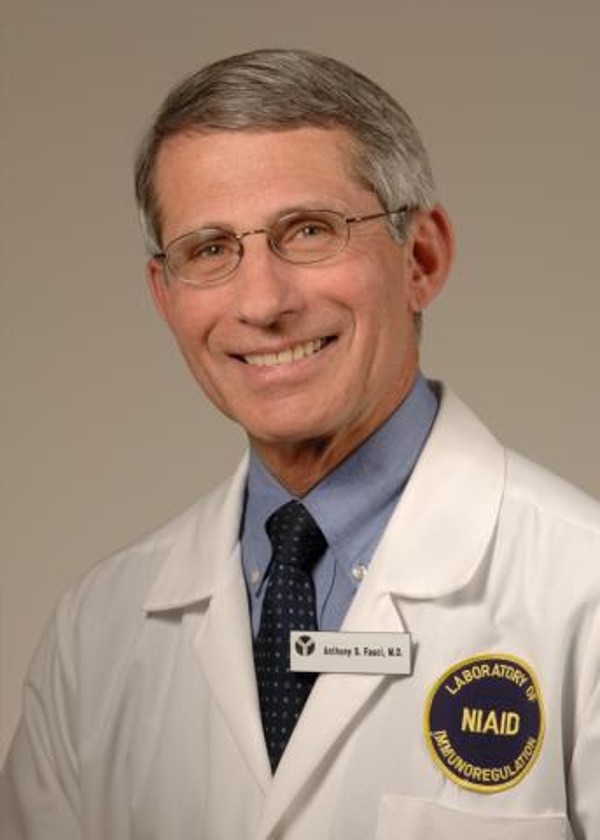
This means that prevention remains “absolutely critical”, according to Anthony Fauci, director of the United States National Institute of Allergy and Infectious Diseases (NIAID), who attended the International Aids Society conference.
There are 19.5 million people on ART today, with another 17.1 million who need it.
“Each year we add about two million to that group,” Fauci said. “We must decrease the number of new infections.”
Scientists outlined five ways the spread of the disease is being curbed.
1. Circumcision.
According to the World Health Organisation, there is “compelling evidence” that male circumcision reduces the risk of sexual HIV infection in heterosexual men. On Tuesday in Paris, researchers said it also protects their female partners.
In a study with nearly 10,000 people in South Africa, women who reported that their most recent male sexual partner was circumcised were 22 per cent less likely to have HIV and 15 per cent less likely to have genital herpes than women whose last partner was not.
The reason is not clear. Is it simply that fewer men are being infected and infecting others in turn, or does circumcision actively prevent HIV-positive men from passing on the virus?
Research will continue, said Ayesha Kharsany of the Caprisa research centre in South Africa.
“What is certain, however, is that having a circumcised partner can provide women with partial protection against HIV,” she said.
Some 12 million men have been medically circumcised in sub-Saharan Africa to date in an effort to stop the spread of HIV, Kharsany said.
2. Antiretroviral therapy
A study of gay couples in which one partner had HIV showed that infected men who achieve virus suppression with ART also protected their uninfected partners.

“There were no, zero, HIV transmissions within these couples,” said Andrew Grulich of the University of New South Wales in Australia, who took part in the study, entitled “Opposites Attract”.
Grulich and a team followed 330 couples for about 18 months, during which time the participants reported 17,000 acts of anal sex without condoms. The lack of HIV spread was all the more notable for the fact that there were high rates of other sexually transmissible infections.
“We think these findings really strongly support the hypothesis that sex [without condoms], when the viral load is undetectable, is a form of safe sex,” said Grulich.

3. Vaginal rings
A two-year study of 96 girls aged 15 to 17 in the United States showed that a vaginal ring treated with the antiretroviral drug dapivirine was safe and easy to wear. The ring is worn constantly, and replaced monthly.
In previous research involving adult women, the ring reduced the risk of acquiring HIV by about 30 per cent, according to the research team. Further study is needed to test whether it also protected girls.
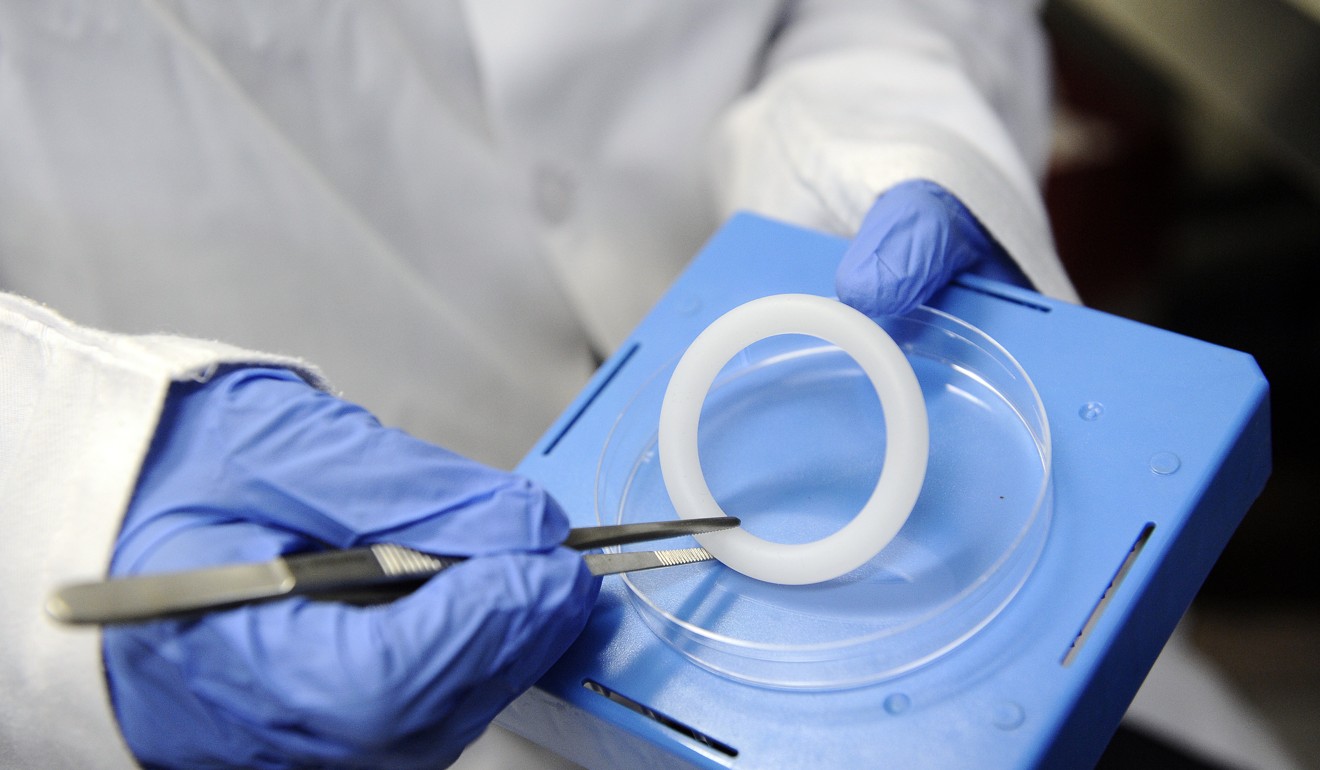
HIV doesn’t distinguish between a 16-year-old and an 18-year-old,” said Sharon Hillier of the University of Pittsburgh School of Medicine in the US. “Young women of all ages deserve to be protected.”
Teenage girls and young women aged 15-24 accounted for a fifth of new HIV infections among adults in 2015, a figure that rose to one in four in sub-Saharan Africa, where 1,000 are infected daily, according to the study authors.
4. Injectable shields
A long-acting, injectable dose of the virus-suppressing drug cabotegravir, given every two months, was well tolerated in trial participants, according to early results.
Cabotegravir is being probed as an alternative to oral antiretrovirals as prevention – and is also known as pre-exposure prophylaxis or PrEP. Forgetting to take a pill can expose one to infection, and is a major complaint of PrEP users.
Further trials are in the pipeline to test the drug’s virus-suppressing efficacy, said Raphael Landovitz, an infectious diseases expert from the University of California.
5. Less frequent sex
A drug cocktail that has been shown to protect uninfected gay men who engaged in frequent and “high risk” sexual behaviour also shields those who are less active and hence take fewer tablets, another study showed.
The trial is testing the efficacy of the drug cocktail Truvada taken as prevention before and after sex.
No infections were reported among men on PrEP who had sex about five times a month, researchers found. The team had previously measured a near 90-per cent drop in infection risk for Truvada users who had sex on average twice as often.

.png?itok=arIb17P0)