Explainer | Arthritis pain can be managed with lifestyle changes, including weight loss, walking and swimming, experts say
- World Arthritis Day helps remind the 500 million sufferers of the most common arthritis type – osteoarthritis – that they are not alone
- Instead of joint replacement, or while waiting for it, experts suggest losing excess weight, having physiotherapy, swimming and taking painkillers

Arthritis is not a single disease; there are over 100 types of related condition that refer to joint pain or joint disease, according to the American Arthritis Association.
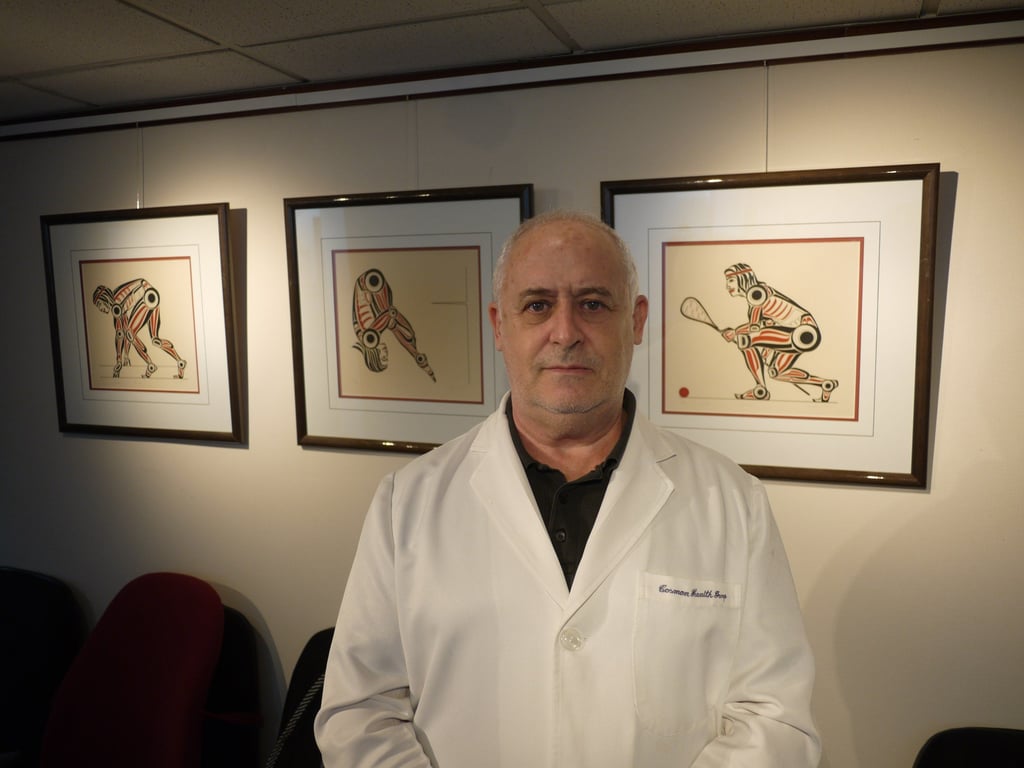
Osteoarthritis – or, as it is sometimes called, degenerative joint disease or degenerative arthritis – is by far the most common, says chiropractor David Cosman at Hong Kong’s Cosman Health Group.
Over time, with wear and tear, joints can become overused or injured and rendered unstable, he says. Key components of joints are damaged, and this can be seen on X-rays or MRI scans.
Breakdown and loss of cartilage in a joint – the stripping away of its cushioning shock absorber – can result in pain from bone grinding on bone. Screening will reveal a reduced joint space.
Where osteoarthritis is a disease of the elderly, rheumatoid arthritis can affect sufferers at any age and is a condition in which the immune system attacks joints, beginning with that important cartilage lining.
Whichever type of arthritis one has, it can be painful: 66 per cent of sufferers report a pain level of 5-plus on a 10-point scale, according to the US Arthritis Foundation, based in Atlanta, Georgia. “That’s moderately strong pain,” it says, “approaching distress.”