Scientists enter new dimension with 4D-printed lifesaving device
Scientists add extra dimension to 3D printing - time - creating personalised device to save lives of infants with severe airway disease that changes shape as they grow
Just when you thought 3D printing – with its ability to produce almost anything from buildings to cars to food – was the coolest thing ever, scientists have taken it another leap forward. Four-dimensional printing is the new black, the added facet being time.
Specifically, 4D printing creates 3D objects that can change shape over time. In the US, researchers from the University of Michigan have managed to print and implant 4D airway splints in three infants with a rare life-threatening airway disease.
The 4D biomaterial was engineered to expand with airway growth over a period of time, before dissolving in the body. In their study published on Wednesday in the journal Science Translational Medicine, the researchers report that the approach has been successful in all three infants with airways remaining open for up to nearly three years after implantation.
“Today, we see a way to cure a disease that has been killing children for generations,” says Dr Glenn Green, Associate Professor of Pediatric Otolaryngology at the University of Michigan.
The findings represent not only a new surgical option for patients suffering from obstructive airway diseases, but also show the promise for 4D-printed materials in medicine.

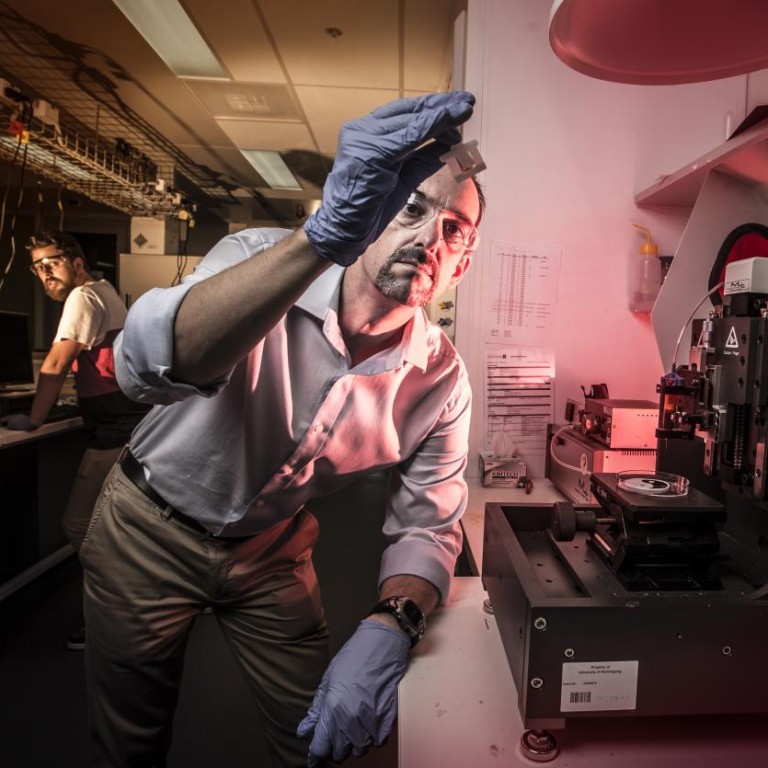
Work by scientists at the University of Wollongong is also helping to set the pace in 4D printing. Researchers from the ARC Centre of Excellence for Electromaterials Science revealed earlier this week a valve that transforms its shape in response to its surrounding water temperature. It closes itself when it detects hot water.
“The cool thing about it is it’s a working functioning device that you just pick up from the printer,” says lead investigator and materials scientist Professor Marc in het Panhuis. “There’s no other assembly required.”
The term 4D printing was coined by computational architect Skylar Tibbits, who runs MIT’s Self-Assembly Lab. He thinks the process could in future be used to build furniture, bikes, cares and even buildings that build themselves. (Imagine adding water to flat-packed Ikea furniture and it assembles itself.)
Instead of lying flat on their backs for weeks on end, these children are now learning to sit and stand and run
In the medical field, recent advances in 3D-printing technology have enabled rapid production of customised medical devices, from hearing aids and dental implants to stents and prosthetics.
However, devices made of rigid material are inappropriate for young patients, often requiring frequent resizing as children grow.
While the Michigan study focused on treating an airway disease, the approach could also apply to orthopaedic, cardiovascular, even gastrointestinal conditions in infants – “anything where you’re expecting a significant increase in either organ or anatomic structural change,” says Dr. Robert J. Morrison, Research Fellow and Resident Surgeon of Otolaryngology Head and Neck Surgery at the University of Michigan.
The infants in the study, between three and 16 months old, had tracheal bronchomalacia, a disease that affects about 1 in 2,000 children around the world. Weakened walls of the trachea (wind pipe) and bronchi (the main passageway to the lungs) in this condition cause airway collapse during breathing, which can lead to respiratory failure and cardiac arrest.

“It's hard to convey how very sick these children were,” says Green. “All of these children had been in the intensive care unit for months. During that time to stay alive, they required heavy sedation narcotics and even paralytics. They all had tracheostomies where a breathing tube was placed through their necks and were on artificial ventilators. They still had repeated episodes that required resuscitations.”
One infant, a 16-month-old male, had been in the hospital since birth.
“There was no cure and life expectancies for each of these children were grim,” says Green. “Now, these children are home with their families. Holidays are not spent in the hospital anymore. Instead of lying flat on their backs for weeks on end, these children are now learning to sit and stand and run as they are no longer sedated and paralysed.”
The researchers say production of the splint took around one to three days, and its material cost was only about US$10. They estimate that on average the children receiving these devices save over US$1 million in medical expenses because they're no longer in the ICU and can get home.
Combining computer modeling, imaging, and 3D printing, the scientists designed the splints tailored to each infant’s anatomy.
The printed splints were hollow and porous tubes that could be sutured over the affected airways and were made of polycaprolactone, a polymer that harmlessly dissolves in the body.
The splint, which lies on the outside of the patient’s natural trachea, stops the collapse of the trachea or bronchi, and is engineered to allow the airway to grow naturally. After the trachea has grown and developed strength and splinting is no longer needed, the splint dissolves.
Today, we see a way to cure a disease that has been killing children for generations
Green says the splint has “worked as intended” and the first infant to receive the implant three years ago as a three-month-old “appears to be cured of tracheal bronchomalacia with the splint that has now functionally degraded".
“If the children are doing well at age three, then we would expect them to do well for the rest of their lives… as long as their airway continues to be able to grow,” says Green.
The researchers plan on pursuing a clinical trial for the airway splint involving 30 children with severe trachea bronchomalacia.
“Three-dimensional printed patient implants as we saw in this case are going to represent a paradigm change in medicine,” says Dr Scott Hollister, Professor of Biomedical Engineering, Mechanical Engineering and Surgery at the University of Michigan, “because cases like tracheal bronchomalacia that may have not have been a large enough market for medical device companies to produce and invest all the money to the manufacturing end previously, you can now do that.”

