Coronavirus: preparing for crisis, hospitals across US struggle under financial strain, equipment shortages
- Medical facilities in smaller American cities and rural areas face grim reckoning as Covid-19 spreads
- Halt in non-essential, revenue-generating surgeries and procedures pummels hospitals’ bottom lines
A Salt Lake City library is churning out 3D-printed face shields. Nurses and medical assistants in Minnesota and Arizona are being asked to take unpaid furlough because of revenue declines. Medical experts in Colorado are preparing to make choices after determining who among their Covid-19 patients they expect will live.
Across America, hospitals and the communities they serve are bracing for the worst as coronavirus cases rise in every state.
As the New York City area announces hundreds of deaths daily, hospitals in smaller cities and rural communities are scrambling to prepare, and in many cases they are already reckoning with the devastating economic crisis the pandemic has caused.
A federal watchdog agency reported on Monday that three out of four of the 323 hospitals it surveyed were treating coronavirus patients. The report painted a grim picture, with a diverse array of problems exacerbated by an insufficient number of beds, tests and personal protective equipment (PPE).
Speaking to The Nevada Independent, health care workers described the eerie, contradictory reality of many hospitals today: hallways silent with most visitors discouraged, procedures postponed and many patients kept in isolation.
And against the background of unprecedented quiet, concern is growing among nurses and other health care workers that they won’t have the supplies to treat their patients and keep themselves safe.
“They’ve been extremely unprepared,” said one nurse in southern Nevada, speaking anonymously.
“Am I going to have enough masks today?” asked one health care provider at a Las Vegas hospital. “Am I going to have to wear this same mask all day whether it’s soiled or not? What is today going to look like?”
That concern was echoed by the American Hospital Association’s senior vice-president of communications, Alicia Mitchell.
“Not a day goes by where we don’t hear from hospitals and health systems across the country that are concerned about shortages of PPE for their heroic frontline caregivers,” she told National Public Radio.
Some unlikely individuals are stepping up to help.
At the University of Utah’s J. Willard Marriott Library, librarians are working with local health authorities to produce 300 medical face shields a day.
“When we first started building our 3D printing programme back in 2013, we had no idea the scale at which our programme would expand and how we would one day play a role that would touch so many lives,” Alberta Comer, the university’s dean of libraries, said in an online newsletter.
Meanwhile, other preparations are under way to manage grave situations that face shields will not resolve.
Trump zigs, zags and zigs again on China and the coronavirus
In Colorado on Sunday, the Governor’s Expert Emergency Epidemic Response Committee called a meeting lasting nearly three hours with its 19 members joining remotely from homes and offices, including one doctor calling in from the front lines wearing a surgical mask.
They met to discuss choices each hoped they would never need to make: how to decide who would receive potentially life-saving treatment if the virus overwhelmed the state’s hospitals.
Under current circumstances, experts warned that Colorado must be prepared to suspend normal hospital decision-making protocols in favour of what are called “crisis standards of care” – carefully delineated triage protocols prioritising treatments based on how sick people are when they arrive, what underlying medical conditions they have and how many years of life they may have left.
For many, the economic fallout from the virus is proving nearly as devastating as the disease itself.
In Minnesota, the coronavirus death toll rose to 24 over the weekend. Yet one of the state’s largest health systems has asked nurse practitioners and physician assistants to volunteer to take a week of unpaid leave starting on Monday.
Feeling the financial strain from non-essential procedures being halted, Fairview Health Services said it was calling on its employees to go on furlough.
Trump wants to defeat coronavirus – and make sure he gets credit
“We’ve moved quickly to slow the spread and preserve necessary equipment by moving a majority of our visits to virtual and postponing all elective and non-urgent procedures,” Fairview officials said in an interview with the Star Tribune in Minneapolis. “The result is not only a dramatic reduction in workloads … but also a dramatic reduction in revenues.”
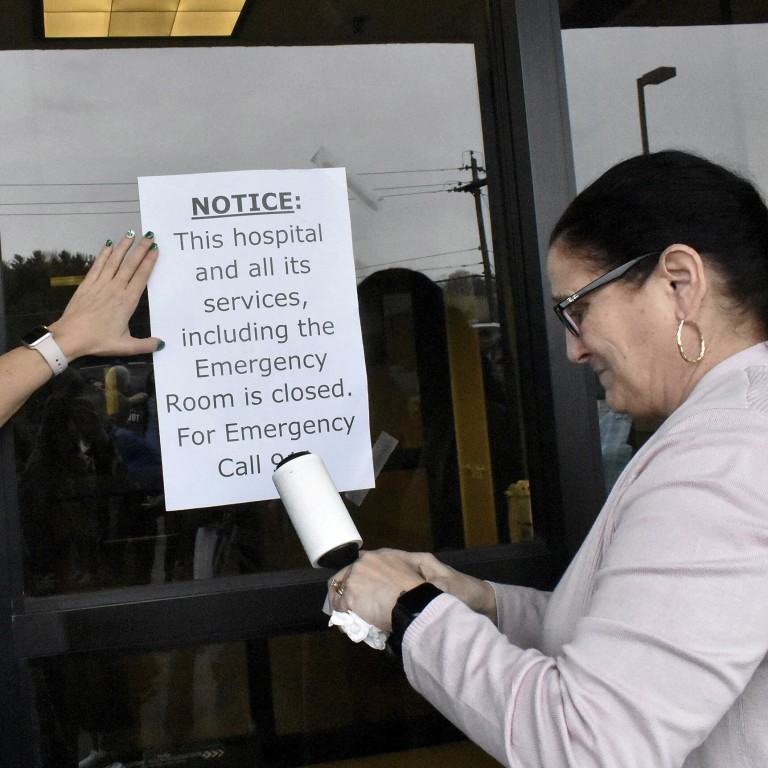
The halt in non-essential surgeries and procedures has medical facilities all over the country feeling the pinch. In Arizona, a small hospital south of Tucson announced over the weekend that it was on the brink of closing because of financial pressure brought on by the coronavirus.
The 49-bed Santa Cruz Valley Regional Hospital must abide by a state order to increase its number of beds by 50 per cent while its income streams dry up.
“We need economic relief to keep functioning,” Kelly Adams, the hospital’s CEO, told The Arizona Republic. “There’s a revenue problem … All hospitals are going to need some economic relief very, very soon.”
The president of the Iowa Hospital Association, Kirk Norris, has warned that many of his member facilities won’t survive the pandemic without cash infusions from the government.
“These community hospitals need cash now,” he said. “They need to keep people in place. They need to stay open. And you can’t lay off half of our workforce. Even assuming we get back on our feet – and they say this is the next six or nine months – there will be hospitals that will not recover from this and will close in Iowa.”
Coronavirus latest: US deaths pass 10,000, Boris Johnson in intensive care
The same pattern is being repeated across rural America.
Last week, on the day its first coronavirus patient was admitted, the CEO of Three Rivers hospital in rural Washington state learned that the facility had only nine days left before it would run out of money to pay its staff and have to close.
Over the course of this pandemic, at least four rural hospitals have closed: two in West Virginia, one in Wellington, Kansas, and one in Carrollton, Alabama.
Even before coronavirus, rural hospitals across the US were struggling to survive, with 126 shutting down since 2011, according to the University of North Carolina’s Sheps Centre for Health Services Research.
Sign up now and get a 10% discount (original price US$400) off the China AI Report 2020 by SCMP Research. Learn about the AI ambitions of Alibaba, Baidu & JD.com through our in-depth case studies, and explore new applications of AI across industries. The report also includes exclusive access to webinars to interact with C-level executives from leading China AI companies (via live Q&A sessions). Offer valid until 31 May 2020.


