
Death should not be a taboo, says Hong Kong doctor who has seen thousands of people die
Long-time staff member at Queen Mary Hospital reminds people not to grieve end of life but to navigate it with right mindset
Medical monitors beep in the background and the pulse of Dr Chan Wai-ming’s patient grows weaker until one last alarm pierces the silence.
In full view of dozens of doctors and nurses inside the intensive care unit at Queen Mary Hospital, Chan, who serves as chief of service in the ward, withdraws care on his dying patient, as it was requested.
Having worked in the ICU ward for more than 20 years, the renowned doctor has seen his fair share of life endings.
Drawing upon his vast experience, he asks simply: “Why is our society so removed from death?”

Chan works at a hospital that sees on average 2,600 people die per year. He notes that “I want you to let me go” is a statement uttered to him on numerous occasions.
The pleas often leave him and other doctors with no choice but to respect their patients’ decisions not to receive any further treatment.
And after encountering end-of-life scenarios over and over, Chan says he understands better what living truly means.
Elderly Hongkongers could have more say in end-of-life care under proposal
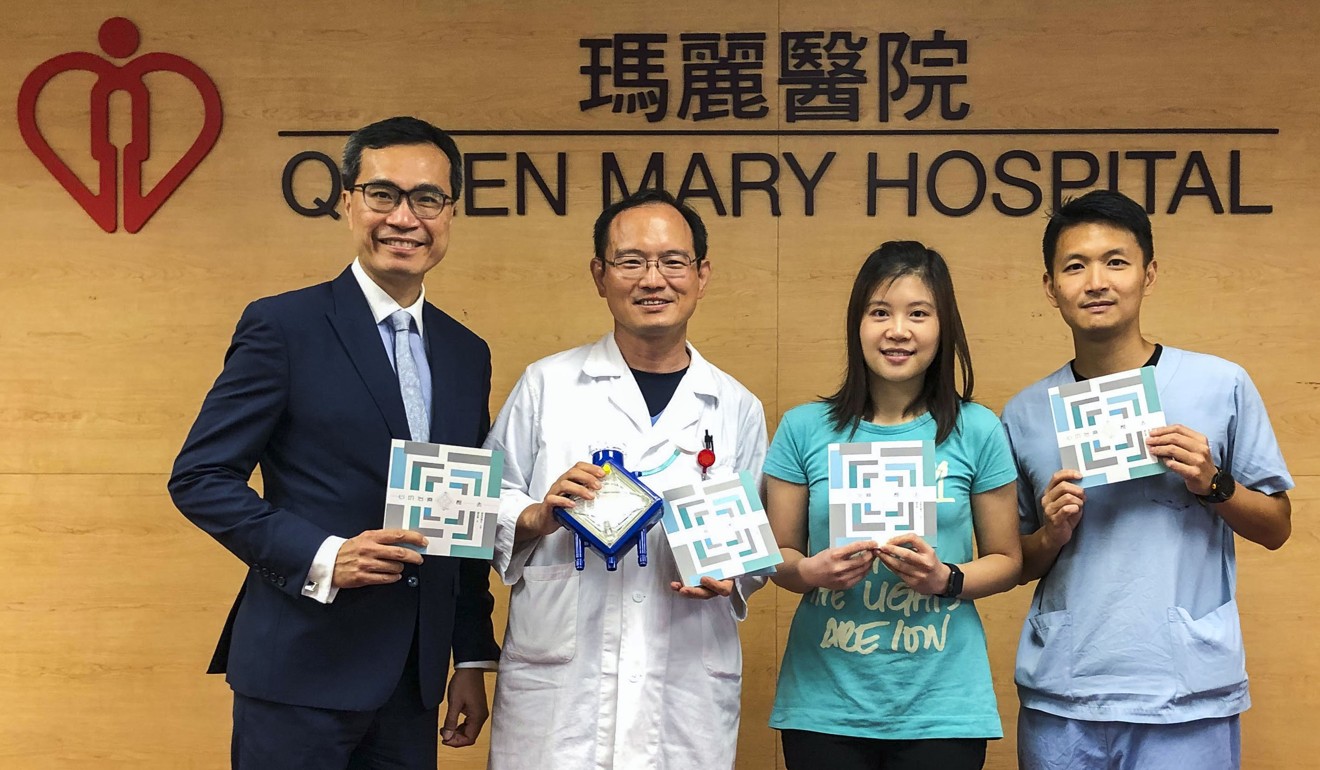
Compiling 16 stories about life and death, the doctor recently published a book called I Care U with Heart: Passing Away. In it, he reminds readers not to grieve but to navigate death with the right mindset.
“Sometimes people would rather die peacefully than have their lives hang on a thread,” he says. “What’s important is how the carers and families cater to the patients during their last moments.”
The odds of living can be stacked against a patient in a place such as the ICU, he adds.

“Sometimes patients aren’t afraid of dying as much as they’re terrified of the suffering that will come with the process of recovering.”
The doctor recalls one case in which he brought a man back from the brink of death after the patient’s condition had deteriorated from acute heart failure. During cardiopulmonary bypass – a procedure in which the functions of the heart and lungs are temporarily overtaken – the patient’s blood vessels narrowed, worsening his circulation and leading to the amputation of his right leg.
While the man did not blame Chan for how things turned out, he did not exactly thank the doctor for saving his life.
Palliative care in Hong Kong and why we need to talk more openly about death
The experience and others like it prompt Chan to question what price one must pay to live.
“I understand that as doctors we save lives to fulfil our obligations, but sometimes we have to ask whether it’s worth it and whether the outcome is something the patient would have wanted,” he says.
The former patient, now in his 40s, is slowly recovering from his heart failure. He relies on a tangle of wires from a ventilator and an IV medication bag by his bedside. For at least the next several months, he will be bedridden, facing countless visits to a physical therapist and the likelihood of using a wheelchair for the rest of his life.
“Without his leg, he won’t be able to drive and for someone who does that for a living, he might have wished to have died instead,” Chan says with a sigh.
The doctor notes that, after discussing in detail their medical conditions, one-third of his patients state a wish to be taken off life-support machines if such equipment is required to care for them.
I wish they had made use of the last moments to say their goodbyes instead of arguing
Amid the grave choices, Chan stays committed to maintaining his professionalism.
“I refuse to let my emotions get in the way,” he says. “Even if there’s a 90 per cent chance of beating the odds, I won’t force that decision on my patients because I would never be able to forgive myself if we did fall into that 10 per cent.”
“There have been times when the patient wanted to pull the plug, but his family members weren’t aware of the request and refused,” he continues. “So the last few hours of that patient’s life were wasted on debates about making the call. I wish they had made use of the last moments to say their goodbyes instead of arguing.”
Advocating improved end-of-life services, Chan sees a need for an advance health care directive, also known as a living will. The document allows a person to specify what actions should be taken for their health if they are no longer able to make decisions for themselves because of illness.
The struggle for Hong Kong’s old and sick to die with dignity
His book is an attempt to get people talking about the issue.
“I hope we can all start by not seeing death as such a taboo topic.”

