Mers breakthrough as University of Hong Kong researchers find combination of two drugs – cyclosporine and interferon – stops virus from spreading
Current treatment for severe infections usually involves the use of interferon or antiviral drugs
University of Hong Kong researchers have discovered a potential breakthrough that could boost survival of Middle East respiratory syndrome (Mers) involving a combination of two readily available drugs.
The combination involves cyclosporine – an immunosuppressant often used in organ transplants to prevent rejection – and interferon, which is used to treat influenza. The drugs would only have to be taken for three to seven days.
Fatty liver disease is the ticking time bomb you’ve never heard of – here’s what you can do about it
Current treatment for severe infections usually involves the use of interferon alone or antiviral drugs.
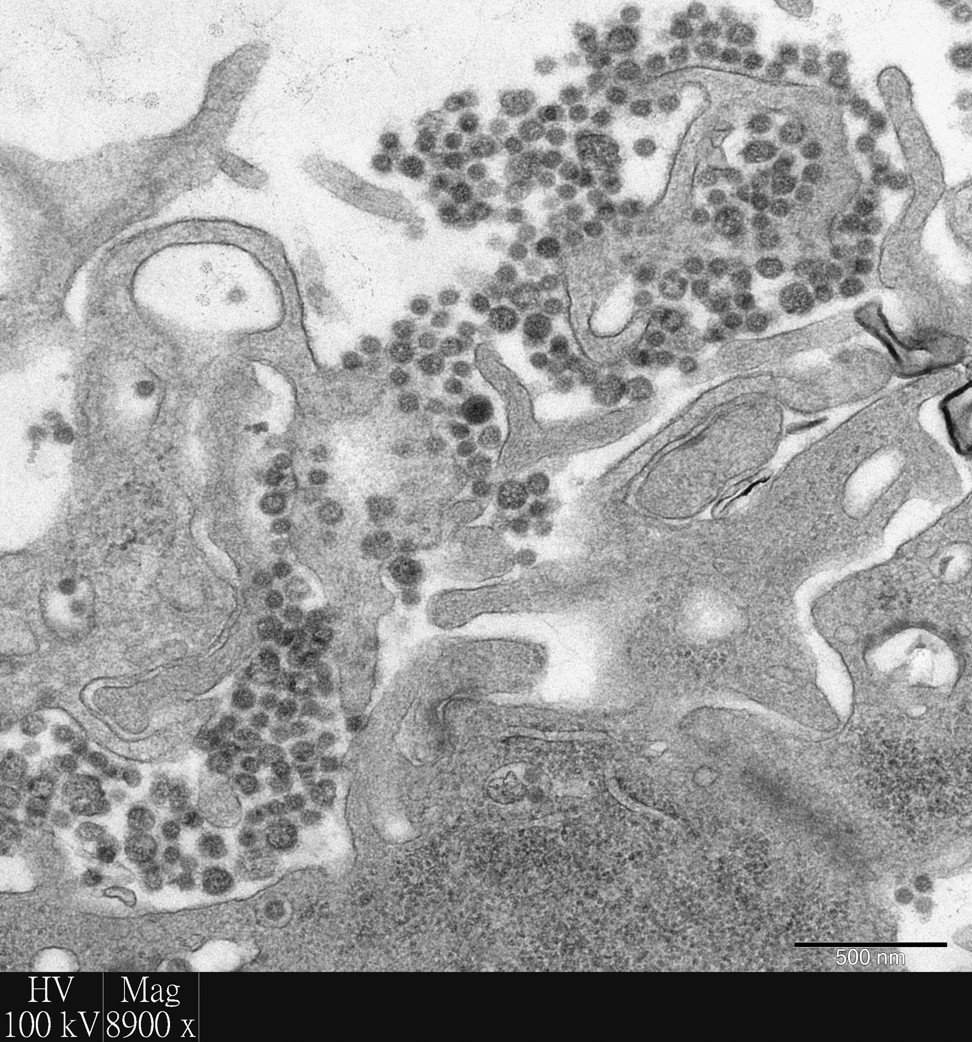
Researchers at the Li Ka Shing Faculty of Medicine at HKU made their discovery using a “lung in a test tube” model they created to study Mers. The model was developed by using discarded human lung tissue from patients at Queen Mary Hospital in Pok Fu Lam.
The World Health Organisation has reported 2,206 confirmed cases of Mers, including 787 deaths – a 35.7 per cent fatality rate – as of April 2018, since it was first identified in Saudi Arabia in 2012.
Heavy-drinking Chinese man contracts rare skin disease
In a study published in the journal, Antiviral Research, the nine-member HKU team led by Professor John Nicholls, showed that “a combination of two currently licensed agents was able to significantly inhibit virus replication and tissue damage by the Mers coronavirus in human bronchus and lung, when compared with single agent treatment or no treatment”.
Nicholls said the study was important because it showed “we have used a combination of two agents which are currently licensed for use in patients with severe infections, such as influenza, and shown the combination ... is really promising compared with a single agent. Clinicians who are treating these patients ... may need to think about using these two agents”.
Why Sars still lingers in the minds of many Hongkongers, 15 years on
Nicholls, in collaboration with Dr Michael Chan Chi-wai, Dr Renee Chan Wan-yi, Professor Leo Poon Lit-man and Professor Malik Peiris at the School of Public Health, developed the model of the human respiratory tract in 2005 in a HK$800,000 (US$102,000) research project.
In camels, Mers is like a common cold so it never goes to the lungs
“As there are few readily available animal models that accurately mimic human disease, it has been a challenge to ethically determine what optimum treatment strategies can be used for this disease,” the team said in Antiviral Research.
Camels are natural hosts for Mers and are the source of infections in humans but are immune to the disease, Peiris said.
Five ways to improve your hospital stay – and help health-care workers help you
“In camels, Mers is like a common cold so it never goes to the lungs,” he said.
Nicholls added: “Since the Hong Kong government wants to promote itself as an innovation and technology hub, we now have the largest series and experience of using this system in the world and are happy to work with companies who are interested in developing new compounds.”