
End of Aids in sight? New medication prevents virus being transmitted
- The study monitored nearly 1,000 gay male couples for eight years, while one partner was HIV-positive and receiving antiretroviral treatment
- HIV and the fatal illnesses it provokes remain one of the world’s largest health crises despite much progress in recent years
An end to the Aids epidemic could be in sight after a landmark study found men whose HIV infection was fully suppressed by antiretroviral drugs had no chance of infecting their partner.
The success of the medicine means that if everyone with HIV were fully treated, there would be no further infections.
Among nearly 1,000 male couples across Europe where one partner with HIV was receiving treatment to suppress the virus, there were no cases of transmission of the infection to the HIV-negative partner during sex without a condom. Although 15 men were infected with HIV during the eight-year study, DNA testing proved that was through sex with someone other than their partner who was not on treatment.
“It’s brilliant – fantastic. This very much puts this issue to bed,” said Professor Alison Rodgers from University College London, the co-leader of the paper published in The Lancet medical journal. Earlier studies have also shown the treatment protects heterosexual couples where one partner has HIV.
She added: “Our findings provide conclusive evidence for gay men that the risk of HIV transmission with suppressive ART [antiretroviral therapy] is zero. Our findings support the message of the international U=U campaign that an undetectable viral load makes HIV untransmittable.
“This powerful message can help end the HIV pandemic by preventing HIV transmission, and tackling the stigma and discrimination that many people with HIV face.
“Increased efforts must now focus on wider dissemination of this powerful message and ensuring that all HIV-positive people have access to testing, effective treatment, adherence support and linkage to care to help maintain an undetectable viral load.”
This powerful message can help end the HIV pandemic by preventing HIV transmission
In 2017, there were almost 40 million people worldwide living with HIV, of whom 21.7 million were on antiretroviral treatment. An estimated 101,600 people are living with HIV in the UK, and of these, about 7,800 are undiagnosed, so do not know they are HIV positive.
Myron S Cohen of the UNC Institute for Global Health and Infectious Diseases at Chapel Hill in North Carolina, said in a commentary in The Lancet on the study that it should push the world forward on a strategy to test and treat everyone who has HIV. But, he added, maximising the benefits of treatment, particularly for men who have sex with men, has proved difficult.
“It is not always easy for people to get tested for HIV or find access to care; in addition, fear, stigma, homophobia and other adverse social forces continue to compromise HIV treatment,” he said.
“Diagnosis of HIV infection is difficult in the early stages of infection when transmission is very efficient, and this limitation also compromises the treatment as prevention strategy.”
According to the National Aids Trust, 97 per cent of people on HIV treatment in the UK have an undetectable level of the virus, meaning they cannot pass it on. “Hearing this can be enormously empowering and reassuring to people living with HIV,” said Deborah Gold, the trust’s chief executive.
Hong Kong’s HIV problem: prejudice is the real malady
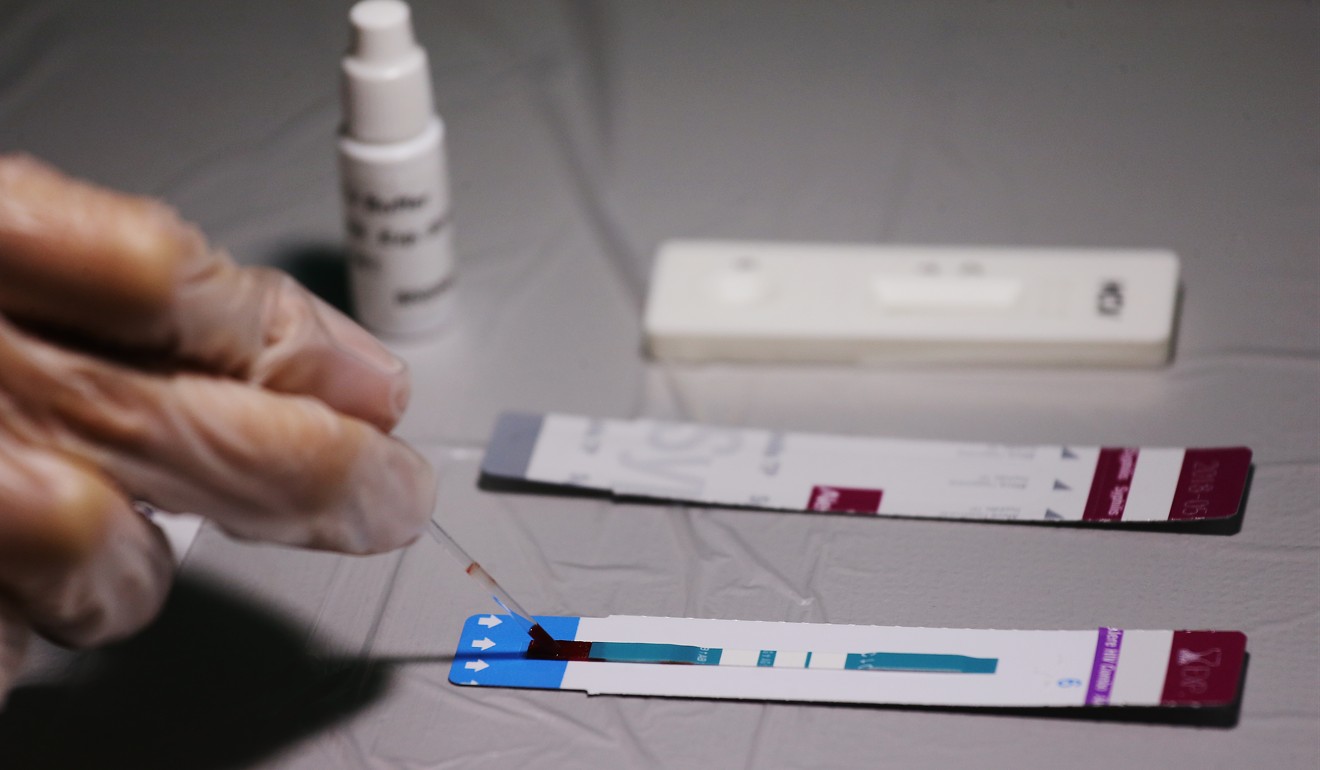
The latest findings reinforce the importance of people taking HIV tests frequently, which could ultimately end the transmission of the virus altogether in the future. New diagnoses have been declining since their peak in 2005, with figures from 2017 showing a 17 per cent drop on 2016 and a 28 per cent fall compared with 2015.
Late diagnosis remains a major challenge, still accounting for about 43 per cent of new HIV diagnoses. This disproportionately affects certain groups, including black African heterosexual men and people aged 65 and older.
“If we don’t reduce late diagnosis, there will always be those who are not aware of their HIV status and who therefore cannot access treatment,” said Gold. “We think that the findings from this study could be incredibly powerful in breaking down some of the barriers to testing in communities where there is still a lot of stigma around HIV.”
However, she added that government funding cuts to specialist health services would make it more difficult to achieve a goal of eliminating transmission by 2030.
Jens Lundgren, a professor of infectious diseases at Rigshospitalet, University of Copenhagen, and joint-lead for the study, called Partner, said: “We have now provided the conclusive scientific evidence for how treatment effectively prevents further sexual transmission of HIV.”
Visa restrictions for HIV-positive immigrants still in place in dozens of countries
Dr Michael Brady, the medical director at the Terrence Higgins Trust, said: “It is impossible to overstate the importance of these findings.
“The Partner study has given us the confidence to say, without doubt, that people living with HIV who are on effective treatment cannot pass the virus on to their sexual partners. This has incredible impact on the lives of people living with HIV and is a powerful message to address HIV-related stigma.”
Bruce Richman, the founding executive director of the Prevention Access Campaign, which launched U=U, said Pac was tremendously grateful to the researchers and participants. He said the study “has forever changed what it means to live and love with HIV around the world”.
In a linked comment in the journal, Cohen expressed optimism for future treatment of Aids. “During the course of these studies, antiretroviral drugs have become more effective, reliable, durable, easier to take, well tolerated and much less expensive,” he said.
“The results … provide yet one more catalyst for a universal test-and-treat strategy to provide the full benefits of antiretroviral drugs. This and other strategies continue to push us toward the end of Aids.”

