Protect your heart, manage your cholesterols

[Sponsored Article]
While the coronavirus pandemic is grabbing all the attention this year as an unprecedented public health crisis, heart disease remains the number three killer of the general population (1). As the community works collectively to ward off COVID-19, we must also not ignore our cardiovascular health.
According to Dr. Adrian Cheong, specialist in cardiology, hypercholesterolemia remains a grave health concern in the developed world. A survey conducted by the Department of Health has shown that 50% of the people in Hong Kong have high cholesterol levels(2), who are at low to high risks to develop coronary diseases.
Cholesterol is a waxy substance found in the blood that is needed to build healthy cells, but too much of “bad” cholesterol, Low-Density Lipoprotein Cholesterol (LDL-C), causes fatty deposits and eventually plaque buildup in the blood vessels. As these plaques grow, they will make it difficult for enough blood to be supplied to vital organs, causing a variety of diseases such as heart attack or stroke. At birth, we have very little cholesterol(3) but the levels get progressively higher and higher as we age(4). How fast our cholesterol levels grow is influenced by genetics, lifestyle and other health conditions such as diabetes(4).

“There’s a proportion of cholesterol that comes from your diet and some manufactured by your own body, because the liver produces cholesterol no matter what. That ratio differs from person to person so the first strategy is to improve your diet. If it still does not come down enough, then consider taking medications,” said Dr. Cheong.
The pandemic has made everyone more house-bound than ever. Interestingly, this can bring both benefits and adverse effects to one’s lifestyle. People who would normally be frequent travellers are now stuck in Hong Kong for months, giving them extra time to focus on their wellbeing such as diet and exercise. Dr. Cheong has seen patients who have made that change with positive results.
“However, there are others who had an exercise routine that got disrupted because of COVID-19. Now they are apprehensive about going out because their pre-existing heart condition might predispose them to the coronavirus. They should find a way to do exercise like taking strolls and walking stairs where there are fewer people. It is important for everyone to not lose track of your own body out of fear of COVID-19 because heart disease is still the number three killer (1) that requires regular maintenance through diet and exercise,” said Dr. Cheong.
Diagnostics and treatments for cholesterol have improved leaps and bounds over the years. While diagnostics used to be more or less guesswork, doctors now have very good equipment that gives excellent imaging into blood vessels.
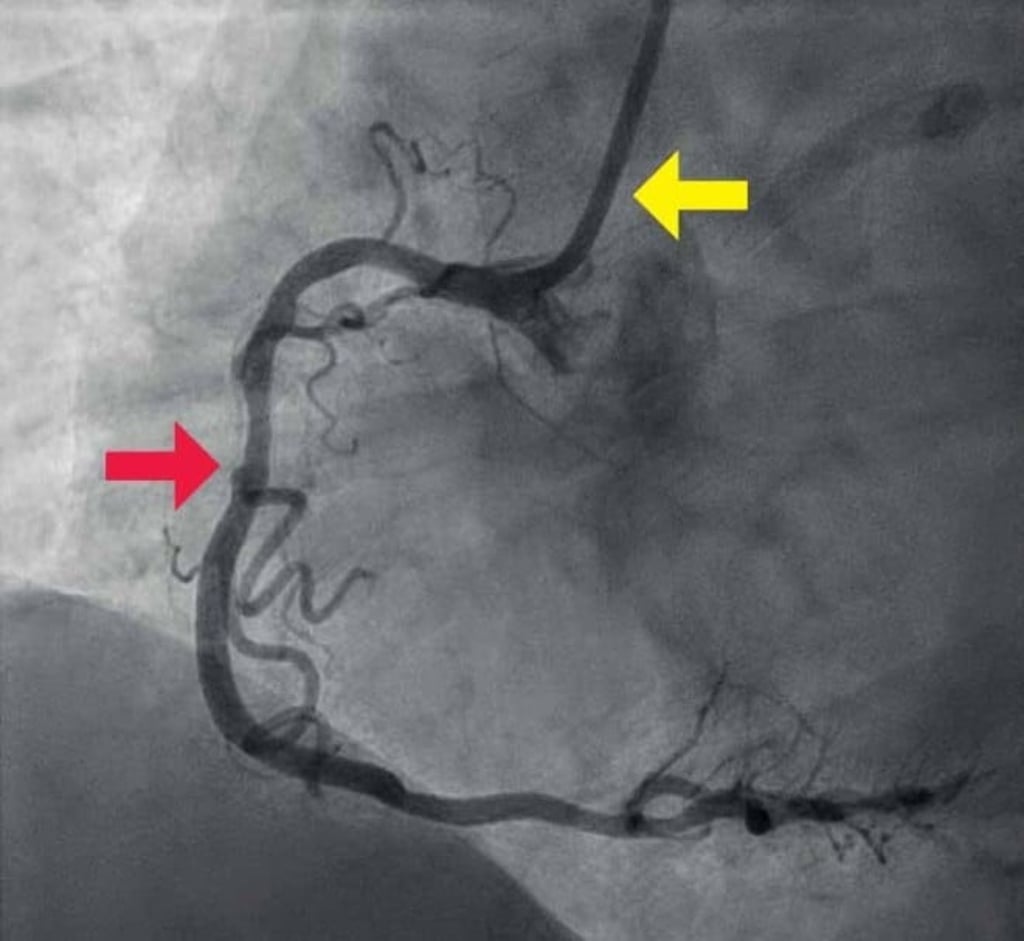
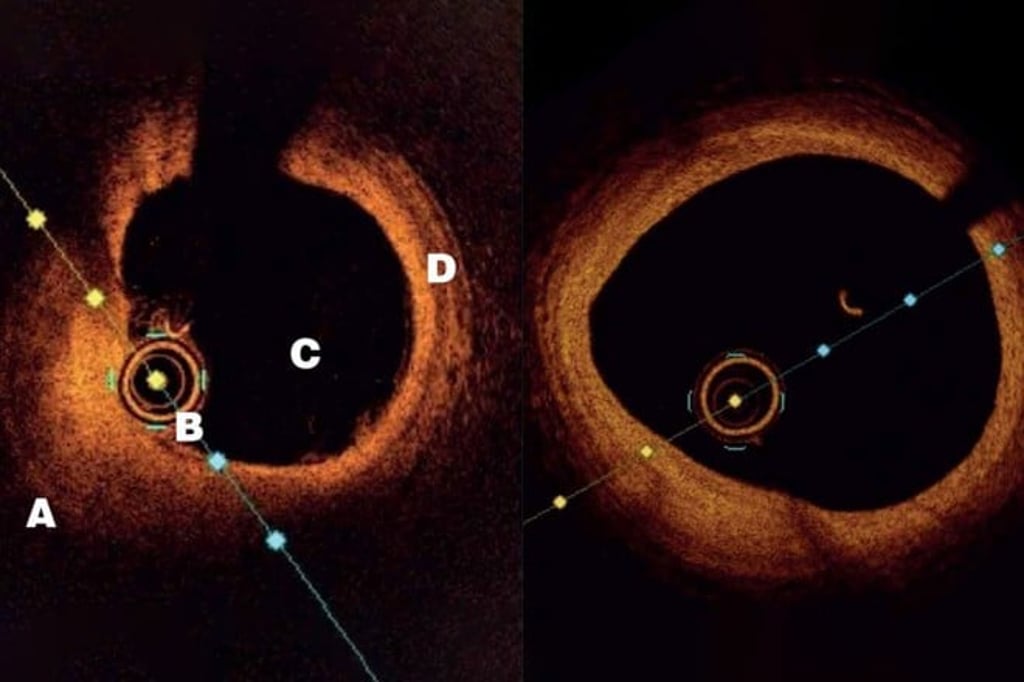
“We can now look at an artery from the inside with HD imagery that shows great details of the plaques. We can see whether they’re old or new, have calcium or are easy to rupture, which greatly improves our diagnostics,” said Dr. Cheong. This advanced imaging technique, called Optical Coherence Tomography (OCT), involves inserting a tiny and flexible catheter into the artery. Using lightwaves near infrared range, OCT allows the doctor to analyse the histology of the plaques(5).
Both surgery and medications are used to treat plaques. In the past, a coronary bypass might be the only option to unblock an artery but now, minimally invasive procedures such as balloon angioplasty or stent procedures have been developed to treat blockages in a safe and effective manner(6).
Traditionally, statins are used to inhibit cholesterol production in the liver but certain people might experience side effects such as muscle pain(7). Now doctors have other options such as NPC1L1 inhibitors and PCSK9 inhibitors(7). On top of statin, often a 50%-65% drop in LDL-C level can be achieved by PCSK9 inhibitors and common side effects include injection site reactions such as pain and redness(7,8). NPC1L1 inhibitors can reduce LDL-C level by 21%-27% additional to statin treatment; common side effects such as fatigue, abdominal pain and diarrhea may occur(7,9). Doctors would prescribe suitable medications according to individual patients’ condition.
“I have a patient who had a major heart attack in his 30s in London in the 2000s. He came to Hong Kong to work and I had to touch up on his stent procedure. Part of his vessels had plaque buildup so I prescribed both a statin and a PCSK9 inhibitor. Three years later, I looked at his artery again and the improvement was remarkable. There was less deposit on the artery wall and his cholesterol was reduced to a very low level,” said Dr. Cheong.
Last but not least, Dr. Cheong advised: "We must now position ourselves to ride the post-COVID recovery - cardiovascular health is a key part of this, and cholesterol is a major risk factor that we can improve relatively easily."
This article is supported by Sanofi Hong Kong Limited. MAT-HK-2000218-1.0-12/2020
References:
1. Centre for Health Protection. Number of Deaths by Leading Causes of Death, 2001 - 2019.
5. Cilingiroglu M, Ozer K. Current Atherosclerosis Reports. 2006;8:140-143.
6. Sousa-Uva M, et al. European Journal of Cardio-Thoracic Surgery. 2019;55(1):4-90.
7. Mach F, et al. Eur Heart J. 2020;41:111-188.
8. Chaudhary R, Garg J, Shah N, et al. World J Cardiol 2017;9(2):76-91.
9. Nutescu EA, Shapiro NL. Pharmacotherapy 2003;23(11):1463-1474.
