Understanding Cholesterol during times of COVID

[Sponsored Article]
COVID-19 has been the hottest topic so far in 2020 and we all are busy with warding off the coronarvirus. While we are drawing most of our attention to the pandemic, have we made enough effort into maintaining our cardiovascular health? Dr. Henry Kok, a specialist in cardiology, pointed out that cholesterol has indeed been triggering a red alert in the developed world and in Hong Kong, nearly half of the population at the age of 15 to 84 has high cholesterol levels(1).
Dr. Henry Kok commented, “There are different researches looking into blood cholesterol levels in different ethnic populations. According to data from the United States, hyperlipidemia is more commonly seen in Whites and Asians, and is less prevalent in Blacks(2). Although dietary intake does affect our cholesterol level, our genetic makeups play an important role in blood cholesterol.”(3)
Surprisingly, the incidence of heart disease in different ethnic groups is as follows – the highest in Blacks, followed by Asians, and lowest in Whites(4). “The reason for such interesting findings is that there are many other risk factors for heart disease including smoking, excessive alcohol consumption, family history and health conditions such as diabetes(5). However, cholesterol is the one that people don’t pay a lot of attention to because we usually won’t experience symptoms of having high blood cholesterol levels.” Dr. Kok added.
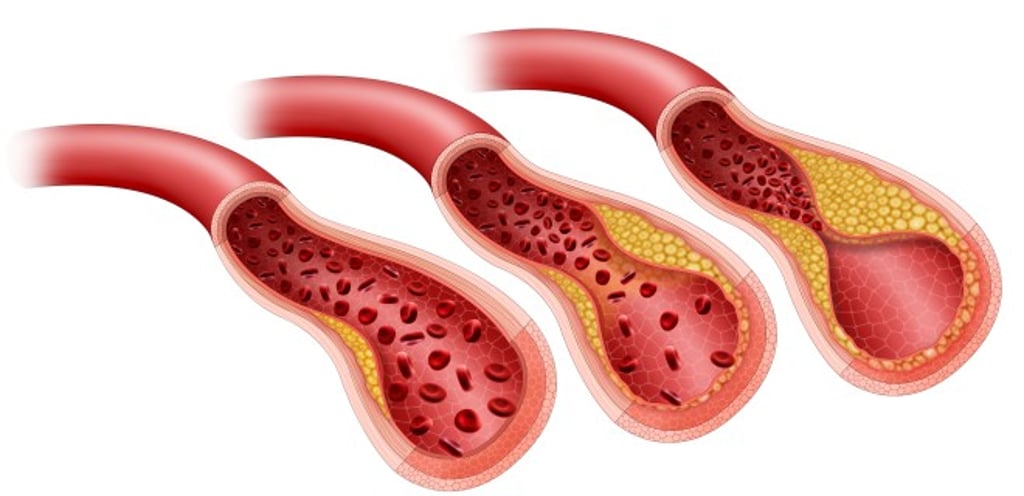
Cholesterol is a waxy substance found in all body cells and our body needs cholesterol for various functions, ranging from producing hormones to transporting fat-soluble vitamins(6). However, too much of “bad” cholesterol, low-density lipoprotein (LDL-C), contributes to the build-up of plaques in the blood vessels. Accumulation of plaques hardens and narrows the blood vessels, which then limits the blood flow to the vital organs. This could result in serious health problems such as heart attack and stroke(6). So, how much is too much? “LDL-C goal should be individualized,” Dr. Kok suggested.
“Before 2004, with intensive lifestyle intervention and medication, we could only bring high-risk patients’ LDL-C level down to around 1.8mmol/L the lowest. It was very impressive if the level dropped from 5-7mmol/L to 1.8mmol/L, as that could achieve a significant reduction in heart attacks, stroke, or even death rates(7). What about lower than 1.8mmol/L? In the 2010s, there were considerable concerns about adverse effects of very low LDL-C levels, for example, hemorrhagic stroke and increase in cancer risks(8). When it came to around 2018, with stronger scientific evidence from larger-scale studies, lower rates of heart attack, stroke and death were, in fact, seen with lower LDL-C levels, without any increase in hemorrhage in the brain nor cancer incidence(9).”
European Society of Cardiology updated their guidelines for lipid management in 2019 – the greater the absolute LDL-C reduction, the greater the CV risk reduction. They revised the definitions for cardiovascular risk categories and set stricter goals for lipid management(10). For example, people with atherosclerotic cardiovascular disease, or diabetic patients with three major risk factors, fall into the very high risk group and their LDL-C level shall now be <1.4mmol/L with at least 50% reduction from baseline(10). “If a very high risk patient still showed blockage in his blood vessels even his LDL-C was already below 1.4mmol/L, then we should aim at a more aggressive LDL-C target for him. LDL-C treatment goals should be customized for individuals, they are not just numbers,” said Dr. Kok.
Statins have been the most commonly prescribed drug for lipid-lowering(10). Doctors would put patients on a cholesterol absorption inhibitor in addition to statin if their LDL target was not achieved. Besides these oral drugs, there is another option available for those who need further reduction in LDL-C, PCSK9 inhibitors. They prevent the degradation of the LDL-C receptors on the liver cells and hence, facilitate the ability of our liver to remove LDL-C from the blood. There is an extra 50% to 60% reduction in LDL-C level on top of statin. PCSK9 inhibitors do not cause muscle side effects like what statins sometimes do. Common side effects include injection site reactions and flu-like symptoms, which are well-tolerated by most of the patients(10).
Tips for healthy living during pandemic
We are staying at home for most of the time recently due to COVID-19 outbreak, which supposedly we should be having a healthier living. However, Dr. Kok got more cases with poorly controlled LDL-C at his clinic during the outbreak. “When patients came back for review, around 30-50% of them were seen with their LDL-C level higher now, compared with their records before the pandemic. On further questioning, I realized although patients took their lipid-lowering drugs as prescribed, they spent less time on workout while ordering takeaways more frequently. These foods are usually high in salts and fats.” Here are some advices from Dr. Kok:
1. Order better-quality food deliveries – low salts and low fats.
2. Try to put some time into aerobic exercises even we have been more house-bound than ever.


“We shall watch out for foods’ nutritional values instead of just focusing on their taste when ordering takeaways. And a 15-minute session of high-knee step-up is a useful example of aerobic exercises that we can do at home. These little lifestyle changes help!”

This article is supported by Sanofi Hong Kong Limited
MAT-HK-2000219-1.0-01/2021
References:
- Hong Kong Information Department. Health & Community. Healthier Lifestyle urged. Published on: 27 November, 2017. Available at: http://www.news.gov.hk/en/categories/health/html/2017/11/20171127_170209.shtml. Accessed 10 December 2020.
- Virani SS, et al. Circulation. 2020;141(9):e139-e596.
- Grundy SM, et al. JACC. 2019;73(24):e285-e350.
- Meadows TA, et al. Mayo Clin Proc.2011;86(10):960-967.
- Agyemang C, et al. Globalization and Health. 2009;5:7.
- MedlinePlus. Cholesterol. Available at: http://medlineplus.gov/cholesterol.html. Accessed 10 December 2020.
- Grundy SM, et al. Circulation. 2004;110:227-239.
- Bandyopadhyay D, et al. J Lipids. 2018;2018:8598054.
- Sabatine MS, et al. JAMA Cardiol. 2018;3(9):823-828.
- Mach F, et al. Eur Heart J. 2020;41:111-188.