Hong Kong should not stint on the medication needed to save lives
Albert Cheng says two recent cases of patients who died because they could not afford the costly drugs underline the need for doctors, not accountants, to decide which medication to prescribe
Time and again, we hear the sad news of patients dying of cancer or a rare disease because they have been denied the best that medical science could offer as they could not afford the costly drugs.
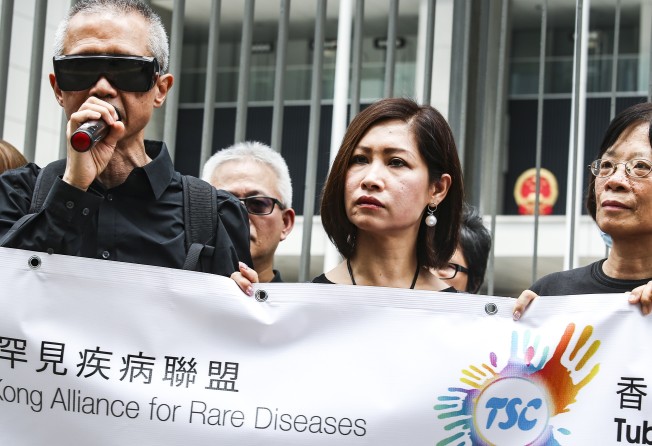
Single mother Chi Yin-lan, 36, had a rare genetic disease and passed away last month, just over a week after her emotive appeal to lawmakers for help. She left behind a 13-year-old daughter who also suffers from tuberous sclerosis complex, which causes tumours to grow in vital organs such as the brain and kidneys.
Chi specifically wanted an expensive drug for her disease to be included in a list of government-subsidised medication.
The government’s pronounced policy is that “no one should be prevented, through lack of means, from obtaining adequate medical treatment”. However, as Chi’s case has shown, this is far from the reality. Even if it is a matter of life or death, there is no discretion. Even if the attending physicians have approved of the use of drugs not on the list, they can only sit on their hands and watch their patients languish away.
Patient groups estimate that less than HK$400 million would be adequate to cover the additional drug bill for the 2,000 or so local patients with rare diseases. In contrast, the government’s budget surplus for last year alone was HK$92 billion.
Fung Kwai-kwan, 77, was another patient who died last week, from prostate cancer, after failing to obtain a new and expensive precision drug. There was no government assistance as the medication fell outside the scope of the current assistance programmes – the Community Care Fund’s medical assistance programme and the Samaritan Fund, both administered by the Hospital Authority.
Fung had sought help through a social worker, but was told flatly that he was on his own. Out of despair, Fung attempted suicide, but was saved. Finally, the NGO Against Elderly Abuse agreed to cover his costs. Unfortunately, it was too late and Fung died five days after he started taking the drug.
Cancer might have killed Fung, but the bureaucratic medical system contributed to his death.
Policies may be rigid, but the people enforcing them should not be. It is vital for the authorities to allow the doctor who best knows the condition of his patient to exercise discretion on prescribing the needed drugs in a critical situation.

Currently, patients who need medication not on the list of subsidised standard drugs must apply for help. Medical social workers will assess their financial status, with reference to their household income, expenditure and capital assets. If approved, a subsidy will be given through the Samaritan Fund.
In early 2011, the Community Care Fund was launched, aiming to expand the safety net to cover more drugs, especially newer ones. It adopts the same financial assessment criteria.
However, this is not enough. The Hospital Authority should give more weight to the expert opinions of the attending teams of medical professionals. If the medical team in charge is convinced that a certain drug not on the pre-approved list should be prescribed, its recommendation should be taken seriously, no matter the cost.
We must not sacrifice patients’ interests in the name of cost control or bureaucratic convenience.
The same principle of empowering the experts to make an ethical call should also apply in organ transplants. The government is poised to consult the public on whether to relax existing rules to allow an underaged person to donate organs for transplant. This follows the case of terminally ill patient Tang Kwai-sze, whose daughter was barred from donating part of her liver to her mother as she was three months short of the minimum donor age of 18. Fortunately, a 26-year-old woman stepped in and donated two-thirds of her liver for a transplant.
Professor Lo Chung-mau, head of Queen Mary Hospital’s liver transplant centre, insists that a definite line should be drawn on the age requirement. There are, of course, two sides to any ethical dilemma. On this matter, I would defer to the experts who know best, including Lo.
Albert Cheng King-hon is a political commentator. [email protected]