
Saying no to total knee replacement surgery: the people who choose exercise and weight loss instead
- New research suggests that cartilage – the cushion that enables joints to move without pain – can be regrown if it gets worn away
- More people than ever are turning to exercises that may help to repair it rather than undergo surgery that entails months in recovery

The burning in his kneecaps was what Richard Bedard noticed first.
Then came the tenderness and pain. Sitting for 10 hours a day as a financial editor in Hong Kong was agonising. So was walking short distances or just standing in the lift.
Neither doctors nor physical therapists could offer any lasting relief. Surgery loomed. But Bedard tried a different approach: an experiment to try to repair the cartilage in his knees with special exercises.
It wasn’t easy and it took more than a year to accomplish, but he sidestepped a knee operation.

Now, 10 years later, Bedard, 57, runs around with his young kids, climbs stairs and bikes up to 60 miles (96 kilometres) on weekends, all without pain. “It was a lengthy process,” says Bedard, who has written an e-book about his successful effort to fix his knees without surgery.
These days, he adds, “I still notice some burning in my knees when sitting,” but for the most part, “my knees feel really good.”
Studies suggest about one in four adults suffers from chronic knee pain. The number of sore, swollen and stiff knees has risen 65 per cent in the past four decades and the increase can’t be explained by ageing or obesity alone, according to the US National Health and Nutrition Examination Surveys and the Framingham Osteoarthritis study.
Knee pain is mostly caused by osteoarthritis. It is the most common form of arthritis and is caused when the cartilage becomes injured and worn, resulting in pain, swelling and stiffness.
Cartilage is the cushion that enables joints to move. But it has no pain receptors, so injuries go unnoticed until much of it has worn away and the joint is damaged. When the knee cartilage is gone and the joint pain is severe – known as stage four or end-stage knee disease – the treatment options are painkillers and total knee replacement, the most commonly performed inpatient surgical procedure for people 45 and older in the United States.
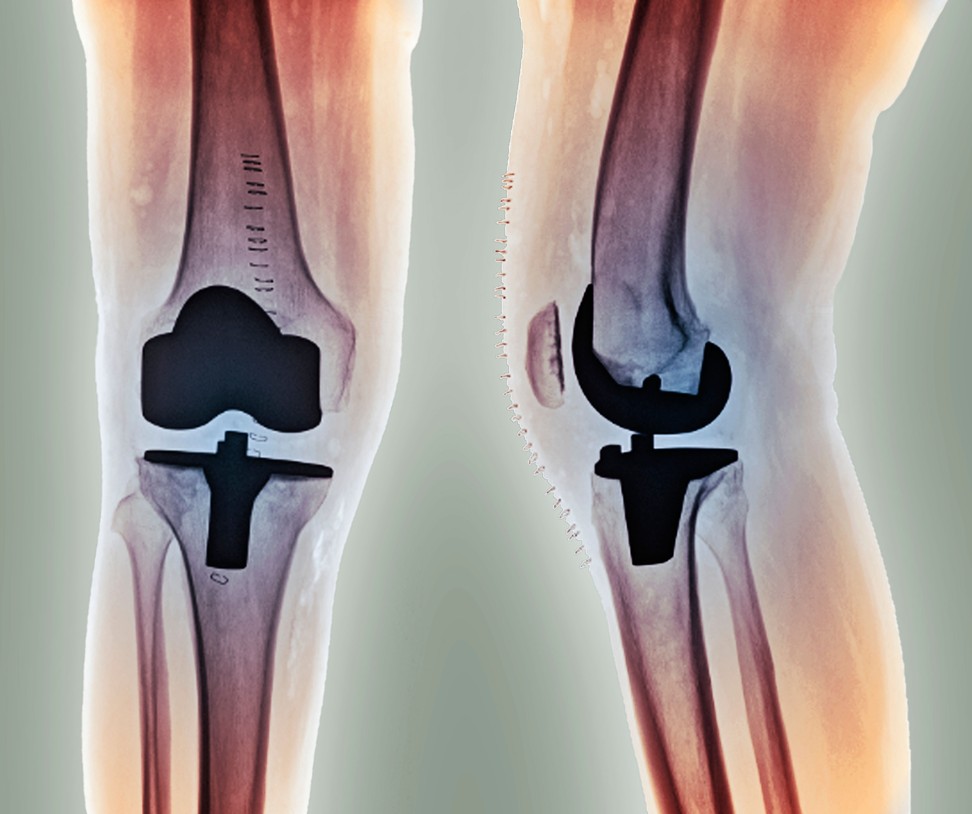
About 680,000 total knee replacements were performed in the US in 2014, according to the National Inpatient Sample, a government survey of hospital patients. Knee-replacement surgery outstrips the 500,000 coronary artery bypass surgeries performed yearly. If trends continue, estimates are that nearly 1.3 million Americans will undergo knee replacement annually by 2030.
While artificial knees can rid recipients of chronic pain and improve quality of life, research suggests that pain persists in as many as 20 per cent of knee replacement patients.
The procedure costs an estimated US$15,000 to perform, requires general anaesthesia and an average of three to four days in hospital, followed by months of physiotherapy.
Once the cartilage is damaged and worn down you can treat the symptoms, but you can’t really make [osteoarthritis] go away
Chronic pain often subsides after recovery, but full range of motion often is not restored.
The range of motion that you “have going into surgery is what you will come out with”, said Elizabeth Matzkin, an orthopaedic surgeon at Brigham and Women’s Hospital in Boston in the US state of Massachusetts, and a spokeswoman for the American Academy of Orthopaedic Surgeons (AAOS). “Knee replacement is done for pain relief, not necessarily to improve range of motion.”
That is why there is strong interest in non-surgical alternatives.

The first line of treatment for osteoarthritis includes the basics: strengthen leg, hip and core muscles, and engage in low-impact aerobic exercise, according to guidelines issued by the American Academy of Orthopaedic Surgeons in 2013.
Weight loss can also help. Every pound shed eliminates four to six pounds of pressure on the knees, according to the AAOS. Over-the-counter and prescription medications can reduce inflammation, but their long-term use also comes with potential side effects.
Those who have early osteoarthritis are most likely to benefit from more physical activity and weight loss. “But it takes time and effort,” Matzkin says, “and a lot of patients are looking for a quick fix.”
Many other treatments are now available, including acupuncture, external braces, dietary supplements glucosamine and chondroitin sulphate, needle lavage, injections of growth factor, stem cells or hyaluronic acid, arthroscopy to repair meniscus tears, use of paracetamol, steroid injections, opioid drugs and pain patches.
Yet, in its 2013 guidelines, the AAOS did not recommend these treatments.
“There wasn’t enough evidence to demonstrate that they are efficacious,” says Matzkin, who served on the committee that wrote the guidelines. Most treatments failed to address the problems of cartilage loss and joint repair, says Matzkin. She says: “Once the cartilage is damaged and worn down you can treat the symptoms, but you can’t really make [osteoarthritis] go away.”

Since cartilage cells don’t have their own blood supply, it has long been thought that these cells could not regrow. But some research suggests that may be wrong.
Among the evidence showing that cartilage can heal is a 2006 study of 325 people.
In the two-year study, 37 per cent of participants showed improvements in cartilage as measured by MRI, compared with 33 per cent whose cartilage worsened.

What separated those who improved from those who didn’t?
Men, younger adults, those with thicker knee cartilage and people who shed more pounds between the first knee measurement and the second two years later were more likely to show improvements in cartilage.
Those who were less likely to experience natural repair of their knee cartilage were women, older adults, people who started with thinner cartilage and those who didn’t lose weight during the two years between the first MRI and the second.
Last month, Duke University, in the US state of North Carolina, reported new evidence showing that cartilage in human hips, knees and ankles can regenerate on its own – in the lab, anyway.
“These new findings suggest a potential for regeneration that might be exploited to enhance joint repair and establish a basis for human limb regeneration”, the team reports in the journal Science Advances. The challenge is that cartilage repair takes a lot of time, since the only way cartilage cells are nourished is by being bathed in joint fluid.
“Cartilage has no direct blood supply, so its ability to use energy to repair itself is very, very slow,” says physical therapist Doug Kelsey, who has written The 90-Day Knee Arthritis Remedy.
Finding the “sweet spot” for injured knees can also be tricky and varies widely from person to person.
It takes just the right amount of movement and weight-bearing pressure to bathe the cartilage cells in joint fluid, allowing them to be nourished and recover without causing more joint damage.
What makes recovery even more complex is that knee pain doesn’t usually surface until hours after an activity, says Laurie Kertz Kelly, a physical therapist and board-certified orthopaedic clinical specialist. “The pain happens later that day or the next day.”
As an example, Kelly points to a client who lived in a three-storey town house. She took the stairs multiple times per day without pain, but then would suffer later.
Kelly advised her to take the steps one at a time with her healthy knee to enable her arthritic knee to recover. That strategy, plus a regimen of weight-bearing exercises that Kelly designed to build up the muscles supporting the injured knee, enabled the woman to recover in about six months.
“Ultimately, she was able to take the stairs the usual way,” Kelly said, and didn’t need knee-replacement surgery.

Richard Sparks, 69, a retired music professor in the US state of Texas, developed “runner’s knee” – a swelling also known as patellar femoral syndrome that makes kneecaps painful. In 2015, Sparks read Kelsey’s book and then consulted Kelly, who worked with him on a leg-strengthening programme that slowly increased the load on his knees.
“It was worth it just to be pain-free so that I can walk and do the things that I want to do,” says Sparks, who recently shed 25 pounds (11kg). He now hikes regularly without pain and no longer takes any knee-pain medications.
“I walk the way I used to walk,” he says. “The longer that I can avoid knee-replacement surgery, the better.”
Is this approach right for everyone?
“All patients that go on to knee-replacement therapy have failed non-operative treatments,” says Matzkin. “I’m not sure that these people are really restoring their cartilage, but they made the symptoms better, and that can absolutely be done with diet and exercise.”