
06:18
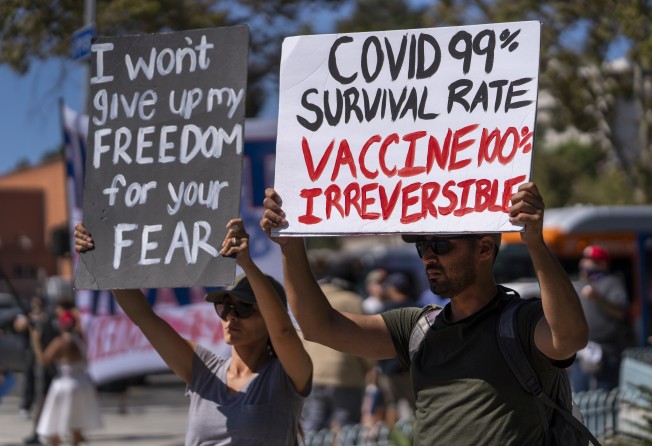
SCMP Explains: What’s in a Covid-19 vaccine?
The United States reached its latest heartbreaking pandemic milestone on Friday, eclipsing 700,000 deaths from Covid-19 just as the surge from the Delta variant is starting to slow down and give overwhelmed hospitals some relief.
It took 3 ½ months for the US to go from 600,000 to 700,000 deaths, driven by the variant’s rampant spread through unvaccinated Americans. The death toll is larger than the population of Boston.
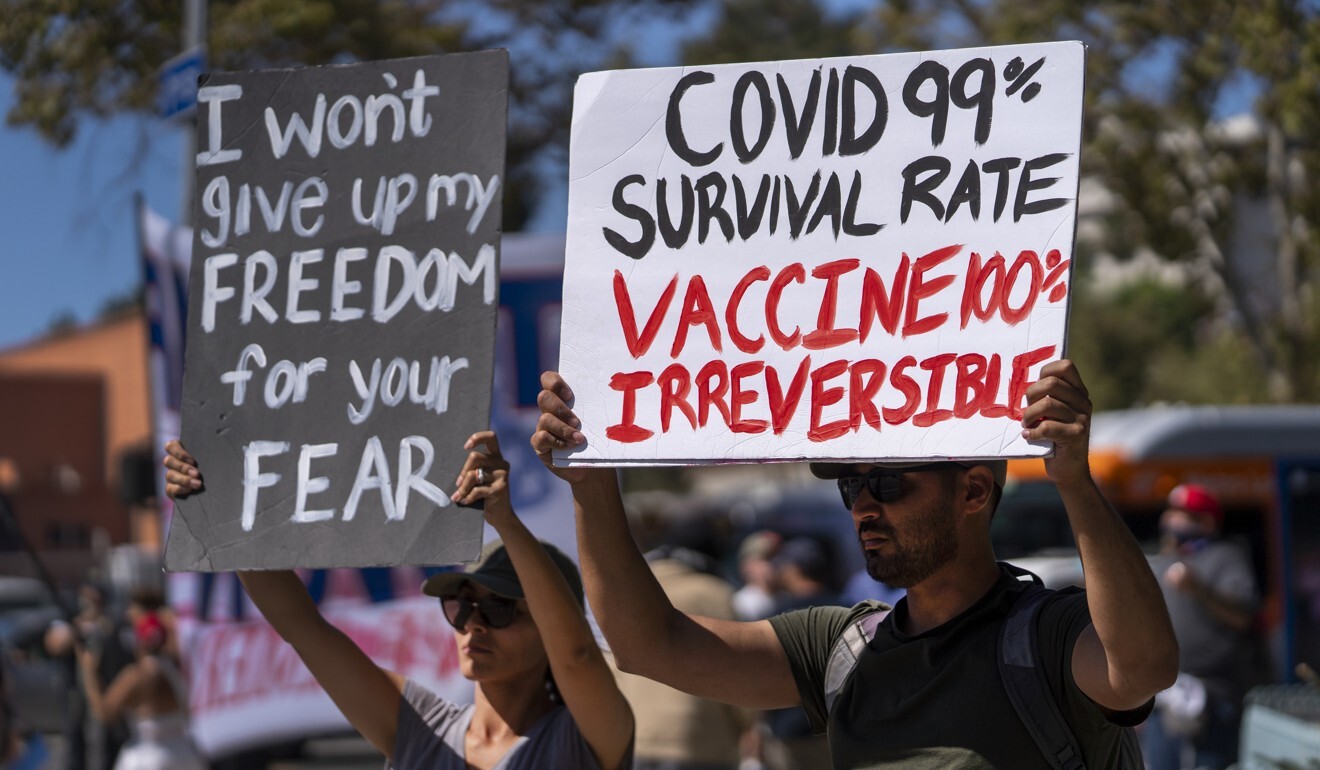
This milestone is especially frustrating to public health leaders and medical professionals on the front lines because vaccines have been available to all eligible Americans for nearly six months and the shots overwhelmingly protect against hospitalisation and death. An estimated 70 million eligible Americans remain unvaccinated, providing kindling for the variant.
“You lose patients from Covid and it should not happen,” said Debi Delapaz, a nurse manager at UF Health Jacksonville who recalled how the hospital was at one point losing eight patients a day to Covid-19 during the summer surge. “This is something that should not happen.”
Despite the rising death toll, there are signs of improvement.
Nationwide, the number of people now in hospital with Covid-19 has fallen to somewhere around 75,000 from over 93,000 in early September. New cases are on the downswing at about 112,000 per day on average, a drop of about one-third over the past 2 1/2 weeks.
Deaths, too, appear to be declining, averaging about 1,900 a day versus more than 2,000 about a week ago.
The easing of the summer surge has been attributed to more mask wearing and more people getting vaccinated. The decrease in case numbers could also be due to the virus having burned through susceptible people and running out of fuel in some places.
Dr Anthony Fauci, the government’s top infectious disease specialist, warned on Friday that some may see the encouraging trends as a reason to remain unvaccinated.
“It’s good news we’re starting to see the curves” coming down, he said. “That is not an excuse to walk away from the issue of needing to get vaccinated.”

06:18
SCMP Explains: What’s in a Covid-19 vaccine?
Unknowns include how flu season may strain already depleted hospital staff and whether those who have refused to get vaccinated will change their minds.
“If you’re not vaccinated or have protection from natural infection, this virus will find you,” warned Mike Osterholm, director of the University of Minnesota’s Center for Infectious Disease Research and Policy.
Our Lady of the Lake Regional Medical Center in Baton Rouge, Louisiana, began seeing a surge of Covid-19 hospitalisation in mid-July, and by the first week of August, the place was beyond capacity. It stopped elective surgeries and brought in military doctors and nurses to help care for patients.
With cases now down, the military team is expected to leave at the end of October.
Still, the hospital’s chief medical officer, Dr Catherine O’Neal, said the rate of hospitalisation isn’t decreasing as quickly as cases in the community because the Delta variant is affecting more young people who are otherwise healthy and are living much longer in the intensive care unit on ventilators.
“It creates a lot of ICU patients that don’t move anywhere,” she said.
And many of the patients aren’t going home at all. In the last few weeks, the hospital saw several days with more than five Covid-19 deaths daily, including one day when there were 10 deaths.
“We lost another dad in his 40s just a few days ago,” O’Neal said. “It’s continuing to happen. And that’s what the tragedy of Covid is.”
As for where the outbreak goes from here, “I have to tell you, my crystal ball has broken multiple times in the last two years,” she said. But she added that the hospital has to be prepared for another surge at the end of November, as flu season also ramps up.
Dr Sandra Kemmerly, system medical director for hospital quality at Ochsner Health in Louisiana, said this fourth surge of the pandemic has been harder. “It’s just frustrating for people to die of vaccine-preventable illnesses,” she said.
At the peak of this most recent wave, Ochsner hospitals had 1,074 Covid-19 patients on August 9. That had dropped to 208 as of Thursday.
Other hospitals are seeing decreases as well. The University of Mississippi Medical Center had 146 hospitalised Covid-19 patients at its mid-August peak. That was down to 39 on Friday. Lexington Medical Center in West Columbia, South Carolina, had more than 190 in early September but just 49 on Friday.
But Kemmerly doesn’t expect the decrease to last. “I fully expect to see more hospitalisation due to Covid,” she said.
One influential model, from the University of Washington, projects new cases will bump up again this fall, but vaccine protection and infection-induced immunity will prevent the virus from taking as many lives as it did last winter.
Still, the model predicts about 90,000 more Americans will die by January 1 for an overall death toll of 788,000 by that date. The model calculates that about half of those deaths could be averted if almost everyone wore masks in public.
“Mask wearing is already heading in the wrong direction,” said Ali Mokdad, a professor of health metrics sciences at the university. “We need to make sure we are ready for winter because our hospitals are exhausted.”