The black fungus nightmare facing India’s coronavirus patients
- Eye-removals and other life-changing operations are taking place around the clock as surgeons struggle to cope with exponential rise in mucormycosis infections
- The fast-moving infection, driven by use of steroids and oxygen in coronavirus treatments, can take hold just days after a patient thinks they have recovered

On being told, on a recent sultry morning in Mumbai, that both her eyes would need to be removed, Neelam Bakshi, 47, could not cry. Her eyes were too stiff, dry, and swollen from the ‘black fungus’, mucormycosis.
“It took a while for my words to sink in. Then she said simply ‘I won’t see my children again’ and went quiet,” said Dr Renuka Bradoo, the specialist treating Bakshi.
The deadly and often disfiguring disease is usually exceedingly rare. But as a second wave of coronavirus infections sweep India, Maharashtra – the state worst affected by Covid-19 – must now cope with an explosion of mucormycosis cases too.
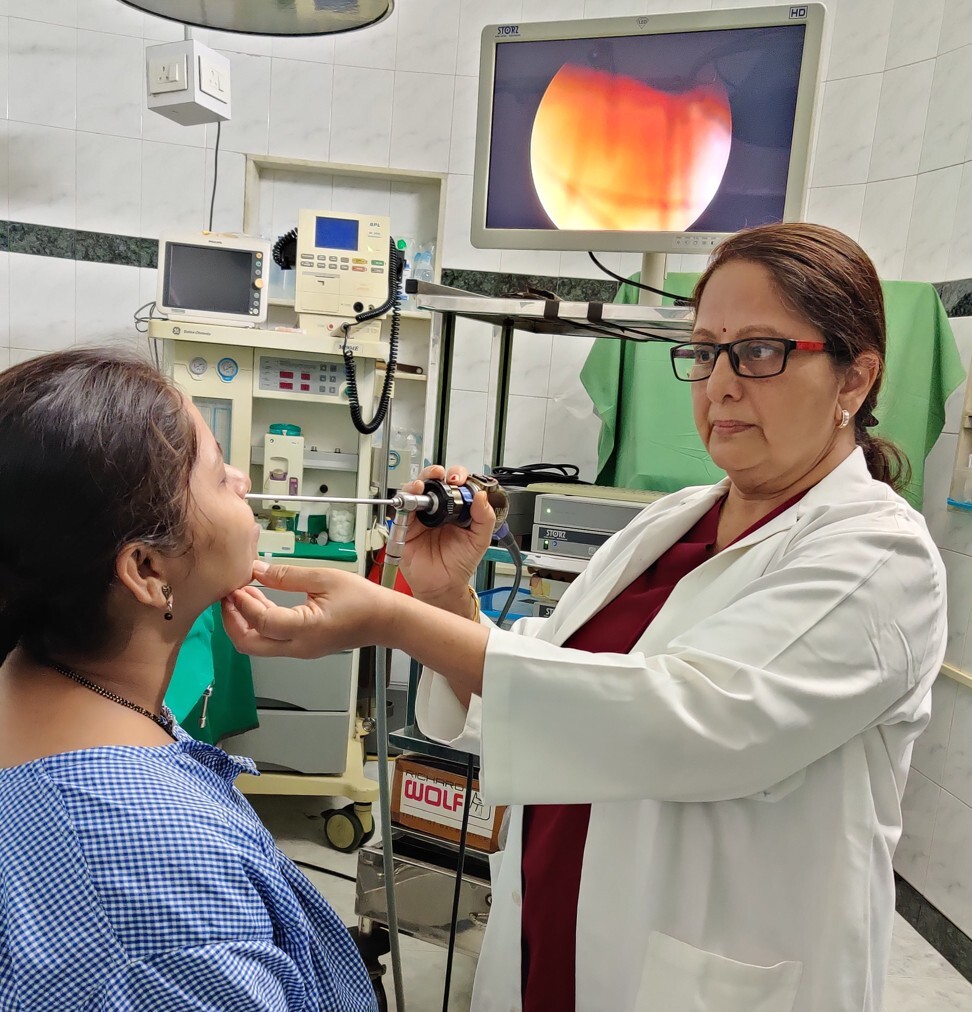
Dr Bradoo, who heads the ear, nose and throat (ENT) department at Sion Hospital, said there had been an “exponential” rise in cases of the fungal infection, calling it “an epidemic within a pandemic”.
Bradoo’s colleague, eye surgeon Dr Akshay Nair, said he had scooped out more eyes than he ever thought possible since the second wave erupted at the start of April. “It’s a nightmare inside a nightmare,” he said.
Normally, mucormycosis affects patients who are immunocompromised owing to uncontrolled diabetes or certain cancers. The current outbreak, though, has attacked Covid-19 patients with diabetes who have been put on steroids to control the virus which in turn has pushed up their sugar levels and compromised their immune systems.

05:35
‘Fear has activated’: How Covid-19 is affecting young people in India
After recovering from the virus, they are discharged and go home only to find, a few days later, one or two strange, but not too alarming, symptoms – a slight discharge from the nose, a headache, a slight numbness in the cheekbone.
The infection starts in the sinuses. In two to four days, it can invade the eyes. If not caught at this stage, it can reach the brain. Since the early symptoms are not too alarming, patients usually consult a doctor fairly late, when they find it hard to open or move their eye. It is often a week or longer before they finally see an ENT doctor who can diagnose it.
By this time, the only treatment is aggressive surgery requiring the removal of one or both eyes or the upper jaw. Once it has spread to the brain, nothing can be done. The mortality rate is 50 per cent.
On May 12, Maharashtra’s Health Minister Rajesth Tope said the state had recorded up to 2,000 cases of mucormycosis.
Speaking from Pune, ENT surgeon Dr Murarji Ghadge, sounded emotionally drained. The outbreak was “rampant and devastating”, he said.
“Last night, I had to operate to remove a patient’s eye at midnight before the infection reached the brain. At 3am I was operating on another patient,” he said.
“Today I will be removing the entire upper jaw and cheek of a young woman. It is mutilating. I have never seen anything like it.”
In neighbouring Gujarat, ENT doctors who previously saw one or two cases of the infection a year are now seeing six to eight cases per day. “My 20 bed hospital has been full of only mucormycosis cases for weeks now,” said Dr Saumitra Shah in Surat.
Dr Nair said that in his WhatsApp chats with six other eye surgeons in other cities, they had noted 58 cases in March. In April, it was 200.
Dr Bradoo said 60 per cent of her patients had needed the removal of one or both eyes. In 30 per cent, the black fungus (a reference to the colour of the necrotic tissue) had spread to the inter-cranial area.
She said that Bakshi barely had time to process the news before having to sign the consent form.
“We have to act immediately before it spreads to the brain. I told her either it’s your eyes or your life. Please understand that removing your eyes is the only way we can get you back to your family,” said Dr Bradoo.
Dr Nair recently removed the eye and upper jaw of a 26-year-old woman who had been severely diabetic for a long time. She can now speak but not eat and is fed through a feeding tube. The disfigurement to the face shatters the patient’s self-esteem. Only many months down the line will she be ready for plastic surgery to reconstruct her jaw.
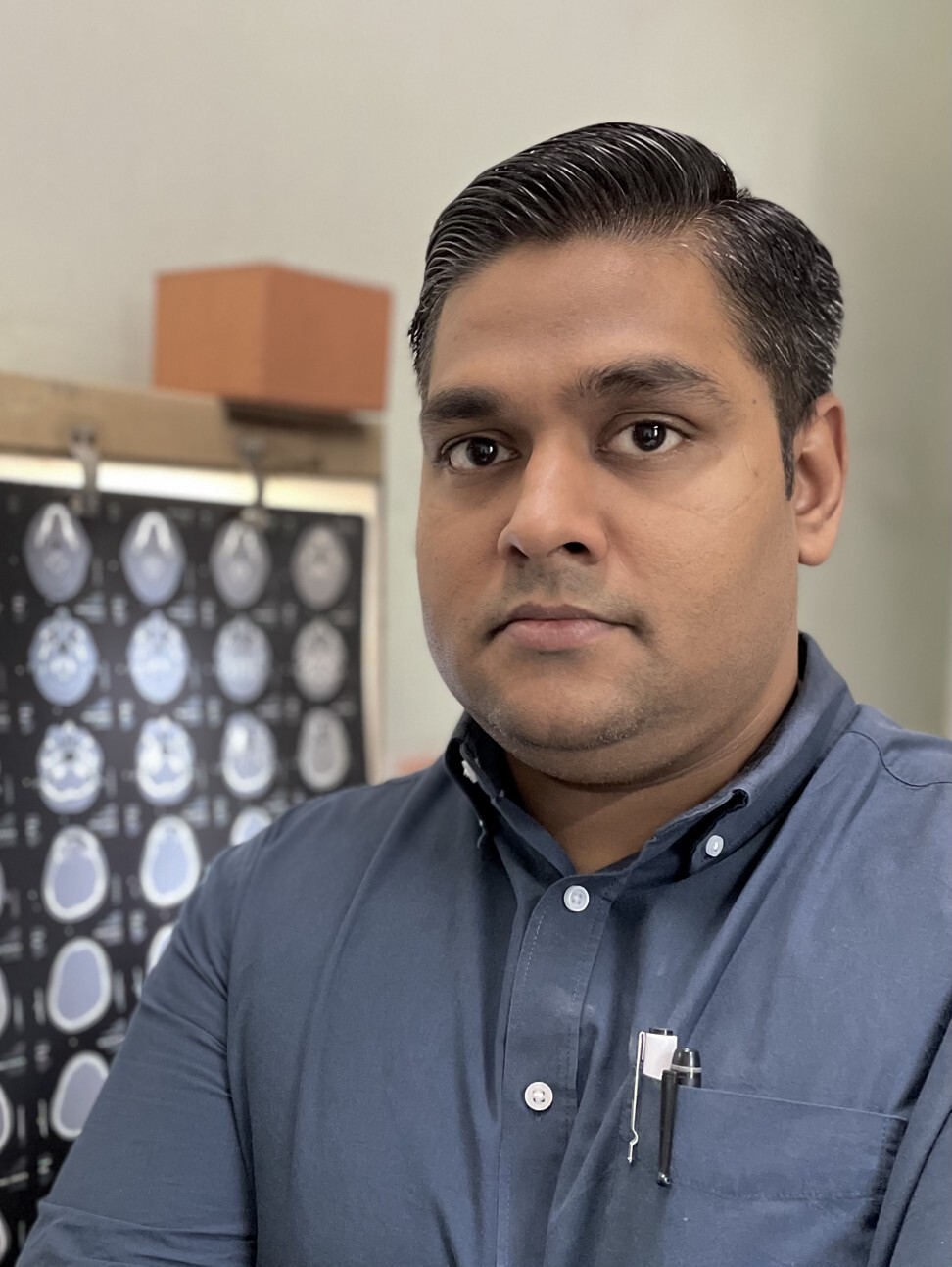
Dr Nair also operated recently on Khurshida Bano, 49, a diabetic who recovered from Covid-19 but had trouble opening her left eye a few days after returning home.
“I had heard of fungal infections after Covid,” said her quick-thinking son Ilyas Ali. “Next morning I rushed her to the doctor who confirmed my fears. By acting quickly, I saved my mother’s life.”
His mother was in a state of disbelief at the diagnosis. “I explained that if an organ goes bad, we need to remove it to save the whole body,” Dr Nair said.
To remove the tiniest trace of the infection so that it could not invade the brain, Dr Nair had to scoop out the entire contents of the bony orbit in a procedure called an orbital exenteration. He removed Bano’s eyeball, tissue, nerves and eyelid.
Talking on the phone from her home in the Mumbai suburb of Bandra, Bano sounded remarkably upbeat. “The moment Ilyas said he didn’t want to lose me and this meant losing my left eye, I understood. Allah has been good to me. My kidneys, heart and lungs are fine … I am getting better,” she said.

At its peak last week, India was recording some 400,000 fresh infections a day for many consecutive days. Public health specialists say the second wave has been different from the first, which began at the end of September, as more patients have been treated with oxygen and steroids for severe Covid-19 cases.
Professor K. Srinath Reddy, president of the Public Health Foundation of India, said the incidence of mucormycosis was lower in the first wave when steroids were not widely used as their usefulness had not been established.
“Now they are standard therapy and while they save lives, they also suppress the immune system. Secondly, more patients this time need oxygen,” said Reddy.
“Many patients are using oxygen concentrators at home. If the water is even slightly contaminated, there is a risk of catching the fungus, particularly in those with suboptimal immunity.”
After the initial treatment, patients face a long hard haul of up to eight weeks. They need very strong and expensive anti-fungal injections.

01:57
Indian volunteers give respectful final farewell to abandoned bodies of Covid-19 victims
The main drug, Amphotericin B, costs around 6,000 rupees (US$80) and each patient needs 50 to 60 injections at the very least. For most people, who have already spent their savings on their Covid-19 treatment, the cost is impossible.
Dr Tatyarao Lahane, head of Maharashtra’s Directorate of Medical Education and Research, who has been seeing “100 times more cases than normal” said that given the scale of the outbreak and the treatment cost, the government would provide free treatment.
Some doctors fear a shortage of Amphotericin B is imminent. “We have told the manufacturers to bump up production quickly. No one expected the surge in demand,” said Dr Lahane.
ENT doctors and eye surgeons have had to hone their counselling skills. “Patients would probably go through the usual cycle of denial, grief, bargaining and acceptance but we have to speed it up. Every minute of delay in operating on them could be catastrophic,” said Dr Nair.
Dr Bradoo had found it “emotionally draining” to tell someone who had perfect vision till a week ago that they were going to lose both eyes.
For Dr Shah, it was the age of some patients that troubled him. “It is disheartening to tell someone in the prime of their life not only that they won’t see again but that they will be disfigured by the removal of their eyes,” he said.