How long will a coronavirus vaccine take? A Q&A with Jerome Kim, head of the International Vaccine Institute
- It normally takes five to 10 years for a vaccine to be approved for market use, but during a pandemic, this timeline may be compressed, says Dr Jerome Kim
- From Britain to South Korea, firms and institutions are working on a vaccine for the Covid-19 disease, offering hope that more than one may be developed
Given the gravity of the crisis, the mission comes with obvious challenges – not least the lack of information on Covid-19, including whether an infected person can build a natural immunity to a second infection.
Dr Jerome Kim, the director general of the International Vaccine Institute and an expert on the evaluation and development of vaccines, tells This Week in Asia about the global race to bring a vaccine to market.

How close are we to a Covid-19 vaccine?
On average, it takes five to 10 years and costs US$1 billion to US$2 billion for a vaccine to reach the final approval to enter the market. There’s a failure rate of over 90 per cent, which highlights how challenging vaccine development is, even for large multinational firms.
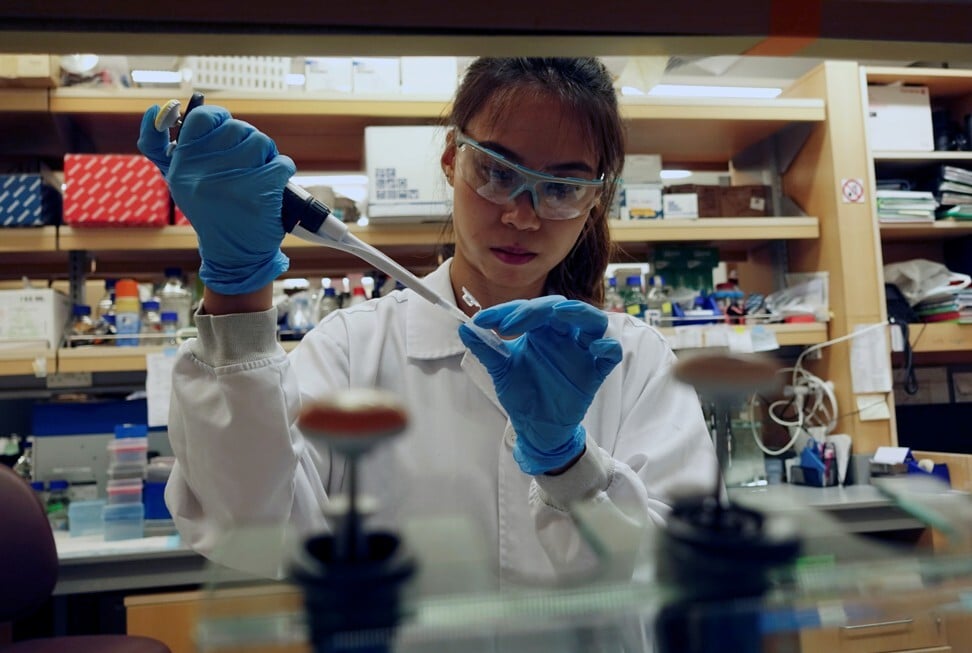
Normally, there are three sequential phases of testing. Phase I is a test of usually fewer than 50 people that looks first at safety and whether responses to the vaccine are found. Phase II goes wider, looking critically at the magnitude and durability of responses to the vaccine. Phase III is the real test of the vaccine’s efficacy and can involve up to tens of thousands of volunteers.
Given the present urgency, Phase I and Phase II of vaccine trials should run together, analysing lab studies and safety in parallel. If a candidate vaccine produces very strong and potentially effective immune responses, the Phase III trial might start before Phase II is complete.
Shortening the timeline has its pros and cons. If a premium is placed on speed, an effective vaccine may be approved sooner – but this approach carries risk. Under normal circumstances, we would have answers to some unknowns before human testing. For Covid-19, we still have some unanswered questions: (a) whether an infected person will be resistant or “immune” to reinfection; (b) whether infection-fighting proteins (antibodies) or killer cells (T cells), or both together, are important in preventing a Covid-19 infection; (c) whether a vaccine can protect an animal against Covid-19; and (d) whether a Covid-19 vaccine will be safe in humans.
David Ho, the man who tamed Aids, in race to find coronavirus vaccine
The gravity of this pandemic, however, compels us to balance safety and speed. Vaccines are given to healthy people, so we cannot compromise on safety. The lack of information on Covid-19 further highlights this responsibility.
Vaccine trials have a data safety and monitoring board (DSMB) that conducts a review at regular intervals. If the DSMB finds evidence that a vaccine offers high levels of protection, it might stop trials to speed the vaccine to approval. Similarly, if it detects signs a vaccine may cause harm, it will stop volunteers from being exposed to risk. The DSMB should monitor participants in accelerated studies for a longer time to ensure their safety.
Is it harder to develop a vaccine for Covid-19 than for other diseases?
An important piece of evidence needed to answer this question is: can a person who has been infected with Covid-19 be reinfected?
There is some information that suggests people who have acquired an infection, and monkeys that have been experimentally infected, can resist a second exposure to viruses. In other words, the immune or protective responses generated naturally by the body can in most cases control, eliminate and protect a person against future infections.
Why there’s no quick fix for a Covid-19 vaccine
This means a vaccine which generates those types of responses should theoretically work, and this holds true for most of the vaccines we use today – including for flu, pneumonia, and the human papillomavirus, which causes cervical cancer. It is harder to develop a vaccine if the immune responses generated by an infection cannot do this – HIV and tuberculosis are examples.
We think Covid-19 falls into the first category, but would be reassured if that were confirmed. If it is, it may be relatively easier to develop a safe and effective vaccine.
What could leaders have done differently to save lives?
Unfortunately, there is no “crystal ball” for pandemics. A country prepares as best it can, but experience clearly helps: Hong Kong’s Sars epidemic and South Korea’s Mers outbreak prepared both for potential pandemics. What’s most important is that we learn from the painful lessons of past outbreaks.
For a country, the first line of defence with an unknown pathogen, like the novel coronavirus, is not a vaccine. It is acute management of the outbreak – establishing control, testing, isolating, tracking and treating – although vaccine work can begin in parallel.
The next coronavirus: the biotech boom boosting Asian defences
The greatest threat in vaccine development is the episodic nature of pandemics. Often, by the time a vaccine reaches human tests, the epidemic has abated.
Funding goes away – even though the threat of future pandemics by the same pathogen remains. This is why despite knowing about Ebola for decades, there were no approved vaccines when the first outbreak occurred in 2013.
Out of these lessons, a collective solution was found. The Coalition for Epidemic Preparedness Innovations (CEPI) – an organisation that coordinates the development of vaccines for emerging infectious diseases – was established in 2017. It is funded by many governments, philanthropic organisations, and global research foundations the Bill & Melinda Gates Foundation and the Wellcome Trust.
When Covid-19 emerged, CEPI quickly provided funding to four groups with “rapid” technologies – one group had designed a potential vaccine within three hours of seeing the virus sequence. By the early summer, these vaccines may be tested in humans. For a process that often takes a decade, it is a persuasive argument for preparedness.
CEPI has secured US$760 million in investments for the Covid-19 vaccine, and says US$2 billion is needed to progress vaccines through development quickly.

Who’s at the forefront of the Covid-19 vaccine race in Asia and beyond?
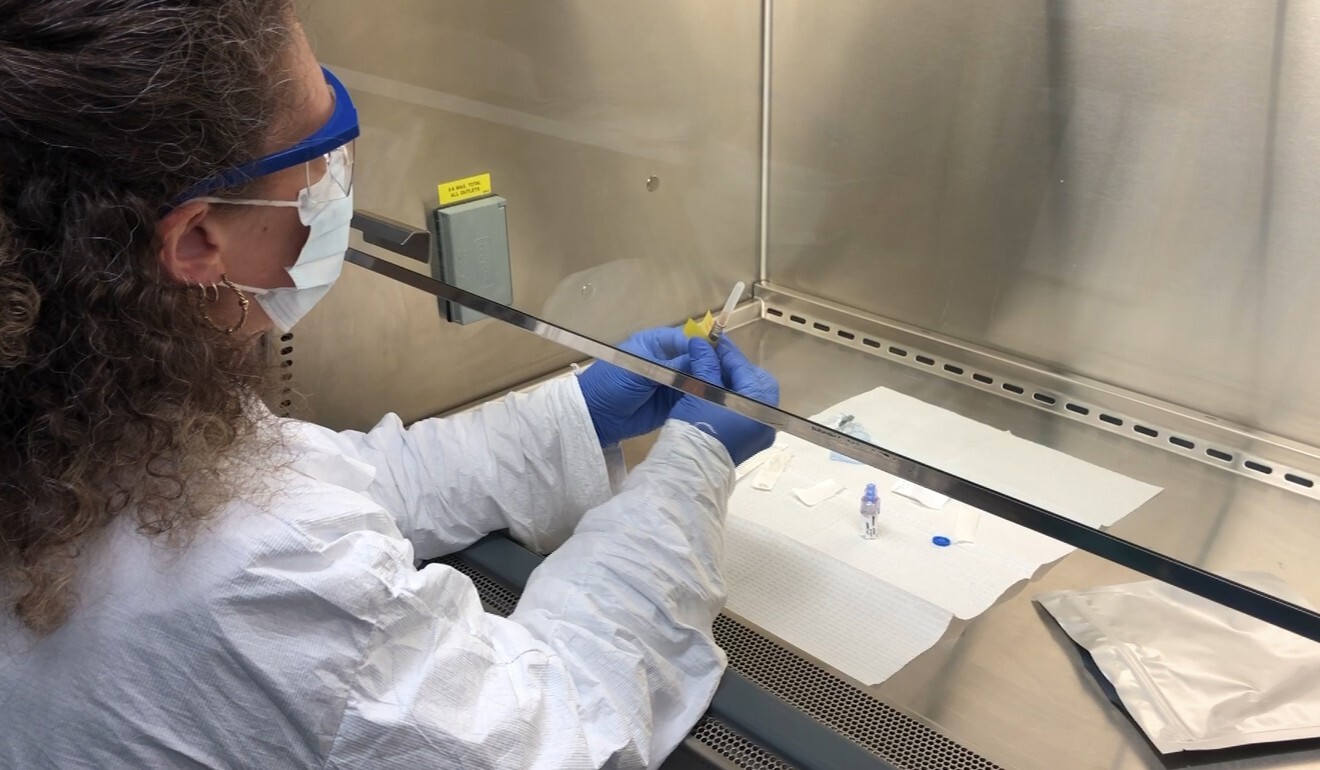
There are now eight small companies and universities – including the University of Hong Kong, German biopharmaceutical firm CureVac AG, and US vaccine manufacturer Moderna – being funded by CEPI to move a vaccine quickly into the first stages of human testing. All candidates chosen had prior examples of vaccines that developed the target immune responses.
The first trial last month of an RNA vaccine developed by Moderna showed it was possible to move quickly into human testing. We don’t know yet whether this or other vaccines will induce the desired immune responses, but the plan is to accelerate all the testing through to Phase II, and, before the end of the year, into Phase III.
What efforts are being made in Asia, including South Korea, to find a vaccine?
According to the Korea Pharmaceutical and Bio-pharma Manufacturers Association (KPBMA), six firms from South Korea – GC Pharma, SK Bioscience, Boryung Biopharma, Sumagen, Genexine and G+Flas Life Sciences – are working on a Covid-19 vaccine. Among these, SK Bioscience plans to start clinical trials as early as September.
The International Vaccine Institute (IVI) is working with a number of companies to fast-track the R&D of the Covid-19 vaccine, including Korean firms Sumagen and Genexine. We are in talks with CEPI, the Korea National Institute of Health, and biotechnology firms to bring a vaccine for testing in South Korea. We have also reached out to universities such as the Baylor College of Medicine in Texas and Britain’s Cambridge University.
South Korean scientists map coronavirus genome, paving way for vaccine
Thai biotechnology Bionet Asia is working with IVI on several potential candidates. These technologies range from nucleic acid vaccines, which contain part of the virus’ genetic sequence to make defensive or immune responses, to a genetically engineered protein vaccine.
All the vaccines are designed to stimulate the body’s immune system to make antibodies and also to stimulate cells that will recognise and kill infected cells.

What are the odds we’ll have more than one vaccine?
Traditionally only one in 10 products that start in a vaccine company’s laboratory becomes a fielded product, so we should be testing a number of candidates initially and determining the ones that will perform the best. In Phase III trials, the companies will propose a use for the vaccines in a “target population”.
CEPI has a mechanism that allows the organisation to look at the data generated for each vaccine candidate and to make rapid funding decisions for the next phases of testing. It would be important for them to negotiate carefully with companies to ensure the vaccines can be accessed by people around the world.
However, it is premature to discuss this since there are yet no vaccines shown to be safe and protective. ■