Coronavirus: lockdown, vaccine, herd immunity. Can there be a winning exit strategy?
- There are many unknowns about Covid-19, but one thing is for sure: every possible way out is riddled with hard choices
- Here are four graphs that explain why
For millennia, many Native American tribes used fire to fight fire by starting small controlled forest fires to clear away undergrowth and debris. Without controlled fires, combustible material accumulates over time until a stray spark starts an unstoppable fire fuelled by all the accumulated debris.
Lockdowns buy precious time but are not a strategy. The immediate fire is extinguished but the population remains vulnerable as large numbers lack any immunity to Covid-19 – akin to a forest-full of combustible material. It will only take a spark.
Exit strategies for Covid-19 must consider this longer perspective, but the following charts explain why there will be no easy solutions and many ethical dilemmas lie ahead.
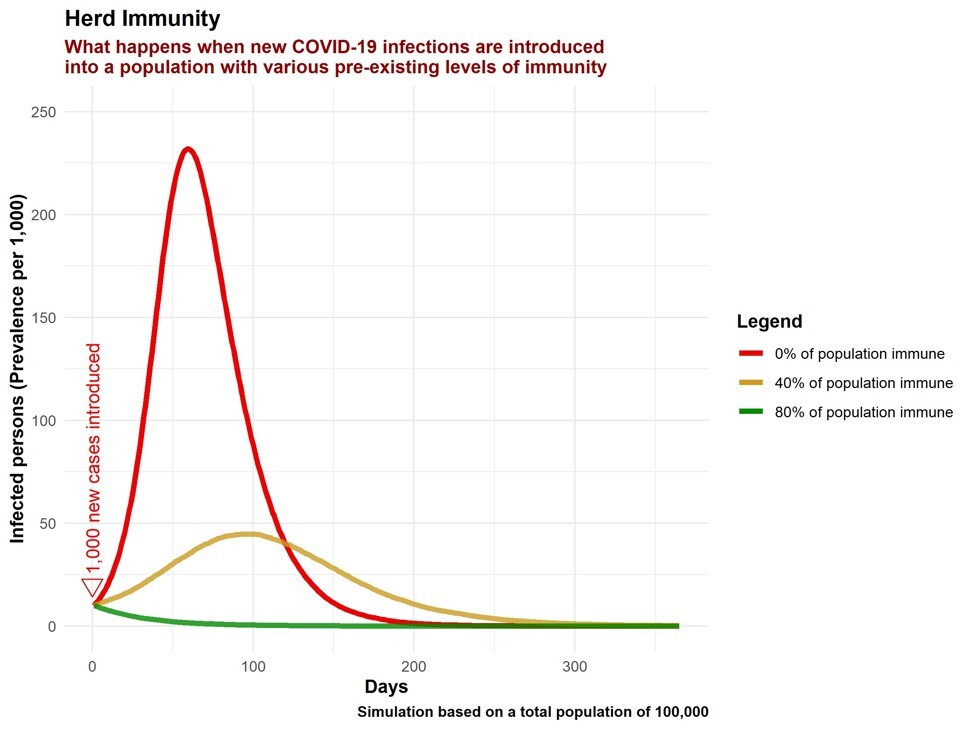
CHART 1: POPULATIONS ‘EXIT’ COVID-19 ONLY WHEN HERD IMMUNITY IS ATTAINED
Lockdowns are not the reason Hong Kong and Korea are beating Covid-19. What is?
Herd immunity is a destination not a strategy. There are two routes to achieve herd immunity – through vaccination or infection – but herein lies the dilemma. The vaccination route could potentially save the most lives, but even if the development of a vaccine can be expedited, testing its efficacy and safety will take a long time and may be unsuccessful. Meanwhile, the route to herd immunity through infection – even if the pace of new infections is controlled by ‘flattening the curve’ – will subject most to the risks of Covid-19 infection.
CHART 2: AN EARLY, ONE-OFF SUPPRESSIVE LOCKDOWN DOES NOT ON ITS OWN SAVE LIVES – IT BUYS TIME TO SAVE LIVES AND LIVELIHOODS
Animated Chart 2 visualises the impressive initial results of a suppression-level lockdown enacted early. Cases will drop to low levels and may even appear to be eliminated. However, this is a lull and not an exit, as the population remains susceptible to Covid-19. On its own, all an initial suppression achieves is postponement of the outbreak with minimal change to the proportion ultimately infected or the height of the peak.
This is already widely understood. A simplistic reopening of the economy without a smart strategy will lead to a surge in cases, if Covid-19 is not fully eliminated. Even if Covid-19 were eliminated locally, it would only take a small spark of imported cases to reignite the outbreak.
Backlash as Malaysian politicians caught flouting lockdown
Yet merely prolonging a lockdown without a strategy has diminishing returns, even as the lockdown locks-in economic damage. At a cost of between one-quarter and one-half of daily GDP per day spent locked-down, lockdowns are among the most expensive ‘purchases’ a country makes. To put things in perspective, in its peak funding year, the Apollo programme cost 0.4 per cent of the GDP of the United States at that time. The share of annual GDP lost from just a week of lockdown, where one-third of potential weekly GDP is lost during that week, would have been more than the share of annual US GDP spent on the ‘moon shot’ in its peak funding year.
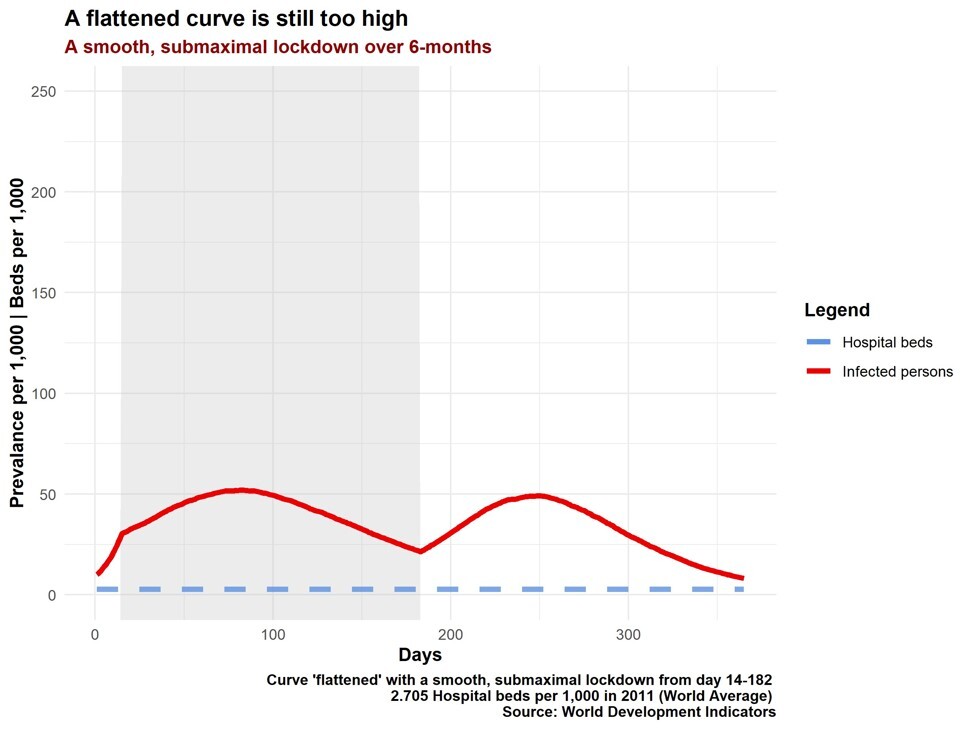
CHART 3: A RELATIVELY ‘FLAT’ CURVE, AIMED AT EXITING COVID-19 BY INFECTION WITHIN 12 MONTHS, WILL STILL OVERWHELM THE HEALTH CARE CAPACITY OF MOST COUNTRIES
However, flat is unfortunately not low enough. With a global average of just 2.7 beds per 1,000, the pre-existing health care capacity of many countries would still be overwhelmed with this relatively ‘flat’ curve. Optimistically, health care capacity can be expanded and adapted to cope with the specific needs of Covid-19. Treatments (such as antivirals) may become available which reduce the health care burden and the risks of Covid-19. Health care capacity is the limiting factor for any strategy aiming for ‘exit’ through the infection route – the greater the capacity used, not just available, the faster the ‘exit’. Countries committed to a Covid-19 exit through infection should make full use of their health care capacity by calibrating measures not to minimise the numbers of daily infections, but to keep daily infections just within health care capacity.
Chart 3 demonstrates another reason for optimism – the lockdown simulated is only needed for half a year and is below maximum intensity. After this, the population attains a small degree of herd immunity and although the outbreak continues, it is subdued and easier to control with minimal social distancing.
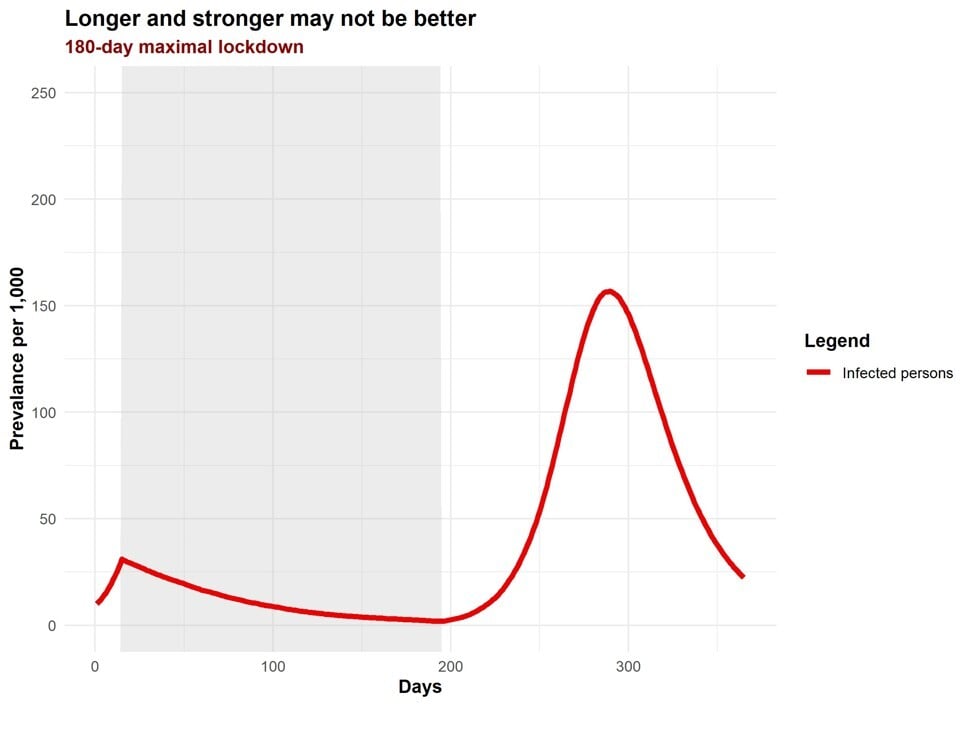
CHART 4: PROLONGED SUPPRESSION FOLLOWED BY ‘GIVING UP’ IS A DEVASTATING EXIT STRATEGY
The route to herd immunity through vaccination is fraught with uncertainty for developing countries with no guarantee if or when a proven vaccine will be available to them. Chart 4 shows the outcome of prolonged suppression followed by ‘giving up’ on all control measures before the population is vaccinated. This would devastate both lives and livelihoods – analogous to investing all resources on suppressing controlled or small fires but ultimately lacking the resources or will to stop the large devastating fire. An early decision to allow a controlled pace of infections, starting with the lowest-risk, to lead to an ‘exit’ through infection would have been less devastating.
Korea’s virus response is the opposite of China – and it’s working
In conclusion, countries have wrenching choices to make to exit Covid-19. The infection route would mean accepting large numbers of infections and deaths from the start, even if the pace can and should be moderated. Some countries with limited health care capacity may not have this option to exit within a meaningful time frame without overwhelming their health care capacity. The vaccination route will hence appear more palatable initially, especially as it is easier to rally a nation together and accept strong measures in the beginning, but as weeks drag to months, the will of any country will be severely tested. The end game needs to be considered, though, as buckling under pressure at a late stage would be devastating.
History is instructive – the 1918-1920 influenza pandemic lasted three years. Of its three peaks, the first was the smallest, the second was the largest. #AvoidTwinPeaks.
Dr Yap Wei Aun is a health systems specialist and adviser to the former Malaysian Minister of Health