
How diet affects brain health and mood, and what to eat to reduce stress and feel good
- Poor diet can damage the brain and impact our mental health, while good dietary habits protect it. A Mediterranean-like diet lowers the risk of depression
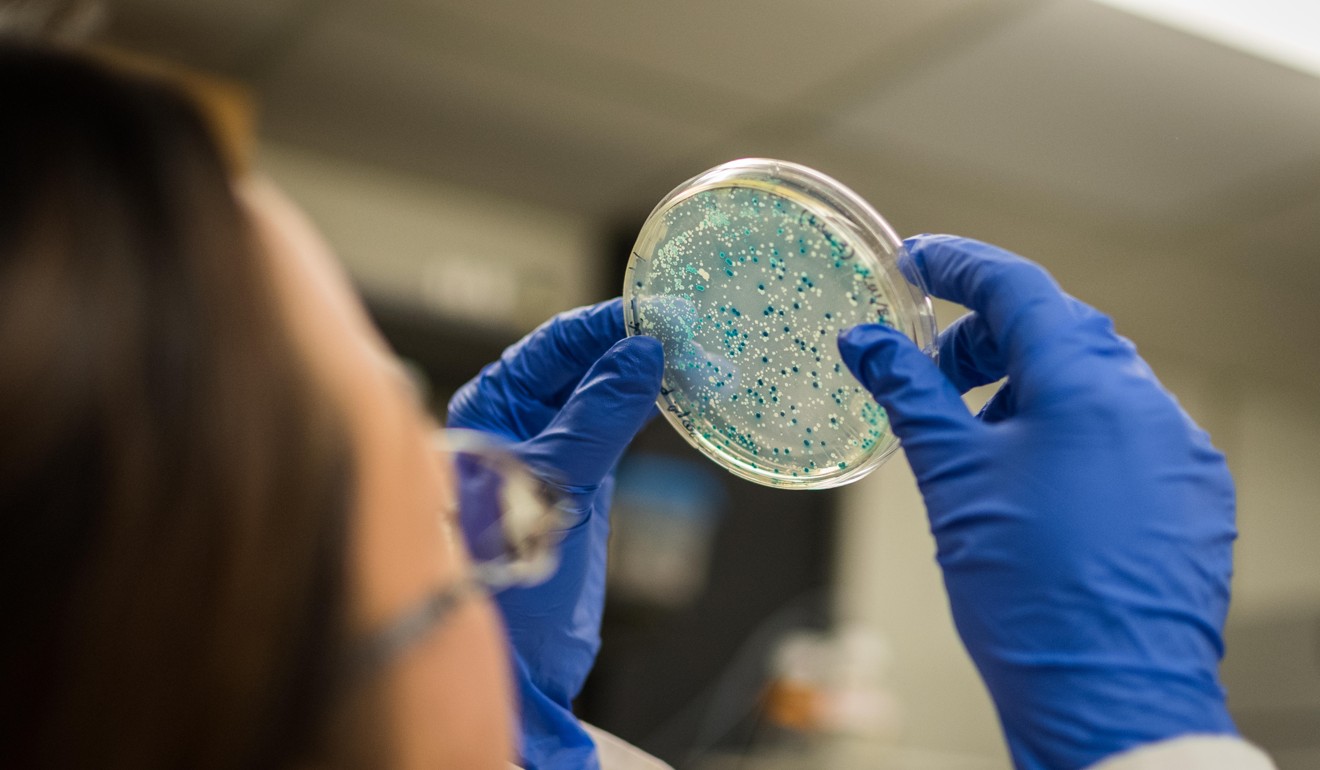
- Gut bacteria break down what we eat, creating molecules that communicate with brain neurons, and can produce antioxidants that head off anxiety and Parkinson’s
In 1829, epicure Jean Anthelme Brillat-Savarin wrote: “Tell me what you eat and I will tell you what you are.” Philosopher Ludwig Andreas Feuerbach echoed the sentiment: “Man is what he eats.” And in 1942, nutritionist Victor Lindlahr published the influential book You Are What You Eat: How To Win and Keep Health With Diet.
In the 21st century, this understanding underpins an entire industry that claims you can eat your way to health. Now a whole new movement is claiming you can eat your way to happiness – and not in the fleeting, temporary way associated with enjoying a slice of chocolate cake.
“Lifestyle interventions are not simply effective – they can be as, sometimes more, effective as drugs in protecting us from depression,” claims Shawn Talbott, a Fellow of the American College of Nutrition and the American Institute of Stress who has written a dozen books on mood state. Talbott advises that people who experience high stress can adopt strategies to manage it. And while he acknowledges that stress and depression are different, he says they are often closely related.
“Chronic stress is frequently a predisposing factor for depression. In fact, many of the ‘anti-stress’ interventions that are effective in reducing cortisol [a stress hormone] exposure will also alleviate depression – eating right, exercising, getting adequate sleep,” he says.
One of the reasons lifestyle interventions are beneficial for sufferers of depression, Talbott says, is because of the multifactorial nature of the illness. He points to research that suggests depression can stem from imbalances, whether this is from a lack of the “happy chemical” serotonin, too much inflammation, a “leaky gut” in which in which bacteria and toxins are able to “leak” through the intestinal wall, or when there are more “bad” bacteria than “good bacteria”.
“If you have a multifactorial problem, you need to address it with a multifactorial solution,” Talbott says. Diet, he adds, is “about as multifactorial as you can get, with thousands of bioactive compounds such as vitamins, minerals and fibre. These can make all the difference in nudging metabolism in the right direction.”

“There is evidence that gut microbes can break down the nutrients we eat and create molecules that may be inflammatory or that may stimulate neural activity. They communicate with the gut and brain neurons and can influence behaviour,” says nutritional epidemiologist Camille Lassale, who works with the department of epidemiology and public health at University College London as well as the Hospital del Mar Medical Research Institute in Barcelona, Spain.
Lassale, who recently published a study into the positive effects of a Mediterranean diet on depression, says poor diet can influence mental health by causing damage to the brain. “This can be due to oxidative stress, insulin resistance, changes in blood flow and inflammation”. On the other hand, Lassale found, a diet rich in anti-inflammatory and antioxidant components, such as those found in oily fish, fruit, vegetables and nuts, can affect the brain by protecting it from stress and inflammation. “This,” she says, “can affect the neurotransmitters responsible for regulating emotion.”
Further studies on animals have found that eating plant-based foods improves the microbial composition in the gut, whereas high-fat diets appear to disrupt it. “These imbalances,” Lassale suggests, “can cause the intestines to become permeable, letting big molecules pass into the bloodstream. These can interact with brain function.”
“The brain can affect the gut, and the gut can affect the brain,” says James Giordano, chief of the neuroethics studies programme at the Pellegrino Centre for Clinical Bioethics, and a professor in the department of neurology at Georgetown University in Washington. “There is evidence that an infant’s gut microbiome can influence brain development, sensitivity to various chemicals from the gut, and even responses to stress.”
The gut can affect the brain in a variety of ways, Giordano explains – for example by producing chemicals that are important in making brain neurotransmitters such as serotonin, which has a role in regulating mood. The microbiome can also contribute antioxidant compounds that can suppress inflammation that might contribute to depression and anxiety, and even neurodegenerative disorders such as Parkinson’s disease.
Five supplements you should consider taking to give your body a boost
Michael Gershon, professor of pathology and cell biology at Columbia University in New York, is the author of The Second Brain. Released in 1998, the book describes nervous conditions of the gut. Gershon agrees that what we eat can affect our mood, “but not much”. He explains: “One of the transmitters in the brain, serotonin, is made in the body from tryptophan, an amino acid. If you eat steak you get tryptophan. The more tryptophan you eat, the more gets into the brain and the more serotonin you make. But you’d need to eat a lot of steak to elevate serotonin noticeably; it wouldn’t be an effective way to change mood.”
While Gershon, who has been nicknamed the “father of neurogastroenterology”, is more circumspect about claims regarding diet and mental conditions, he says it is clear that gut health can directly influence mood.

“When I was at med school we were taught that ulcerative colitis was a personality disorder,” Gershon recalls. “Of course we know now that it is an autoimmune disease and has nothing at all to do with personality. The personality – the resultant low mood – was due to the discomfort in the gut.”
Emeran Mayer, a gastroenterologist, neuroscientist and professor in the departments of medicine, physiology and psychiatry at the David Geffen School of Medicine at University of California in Los Angeles, is a pioneer of medical research into brain-gut interactions. He says that broader acceptance of the concept of interactions between the brain and the gut in the medical community is leading to a renewed interest in diet in the treatment of mental health disorders.
‘A little of what you fancy’ approach to eating is best, say experts
One plausible mechanism, says Mayer, for how diet can influence depression has to do with the activation of the gut-based immune system secondary to increased “leakiness” of the gut which Talbot cites. In leaky gut syndrome, Mayer explains, the end products of dysfunctional gut microbes enter the circulation and reach the brain, disrupting brain chemistry and function.
But how much impact can a change in diet really have on the clinically depressed?
Both Mayer and Lassale refer to the Smiles (Supporting the Modification of lifestyle in Lowered Emotional States) trial, led by Professor Felice Jacka, director of Deakin University’s Food and Mood Centre in Australia. This study, says Lassale, “was the first to provide evidence that diet can affect depression. People suffering depression allocated to the Mediterranean diet group improved their depressive symptoms after 12 weeks, to a greater extent than the control group who received social support.”

A year later, Lassale and Jacka co-authored a review that included 41 earlier studies. Describing the findings in The Conversation, an independent source of news and views from the academic and research communities, Lassale writes, “four specifically looked at the link between a traditional Mediterranean diet and depression over time on 36,556 adults. We found that people with a more Mediterranean-like diet had a 33 per cent lower risk of developing depression than people whose diet least resembled a Mediterranean diet.”
The New York Times bestselling author Dr Mark Hyman, director of the Cleveland Clinic Centre for Functional Medicine, says: “We’re not saying that diet is the solution to healing depression, but it is one important piece of the puzzle. Exercise, stress management, community, purpose, meaning, therapy, and more are all important parts of managing depression.
“People are often looking for that magic bullet that will solve their ailment, and typically, there isn’t one. What I advocate for instead is a comprehensive approach that addresses the mind, body, and spirit.”

