Explainer | What is inflammation? Causes, types, symptoms, treatment for chronic cases, and its link to cancer and autoimmune diseases
- Inflammation is a process that helps the body fight infection and injury, but unchecked, it may trigger autoimmune diseases and other serious illness
- Experts’ advice on dialling it down includes replacing processed foods with immunity-strengthening whole foods, managing stress, and getting exercise and sleep
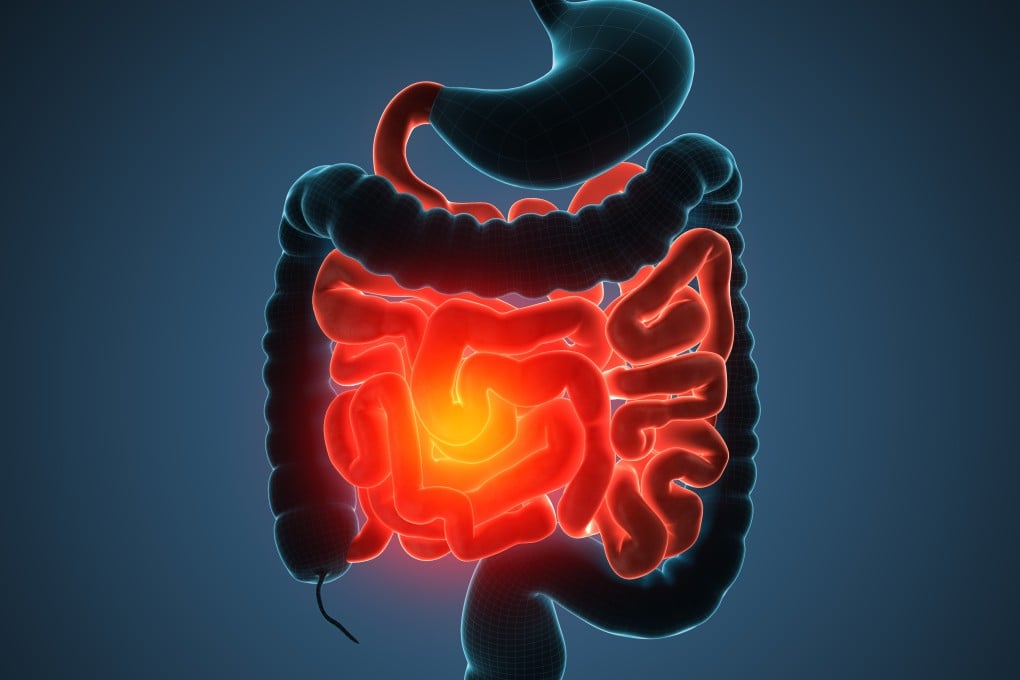
Heart disease, type 2 diabetes, Alzheimer’s disease and cancer are all serious conditions that share a link with chronic inflammation.
Inflammation isn’t actually a bad thing – it’s when acute inflammation doesn’t resolve and becomes chronic that it starts to have a negative impact on our health.
“We need inflammation to fight infections and injuries,” says Maxi Schoenteich, an osteopath and functional medicine practitioner at Integrated Medicine Institute in Hong Kong. “However, when inflammation does not stop and persists beyond the initial infection or injury, we run into problems.”

Some of these molecules travel through our body to our brain to trigger an increase in body temperature – this explains why we get a fever when we have a cold or flu.
A higher body temperature makes it more difficult for viruses and bacteria to survive; the fever, aches, pain and brain “fog” that you experience during a cold or flu aren’t actually caused by the virus, but by your immune system, to fight the infection and force you to stay in bed and rest.