100 years of insulin: the history of life-saving discovery that changed the treatment of diabetes forever
- On World Diabetes Day, the Post’s Simon O’Reilly – a type 1 diabetic – explains how insulin works and the milestones that saw it become widely available in 1923
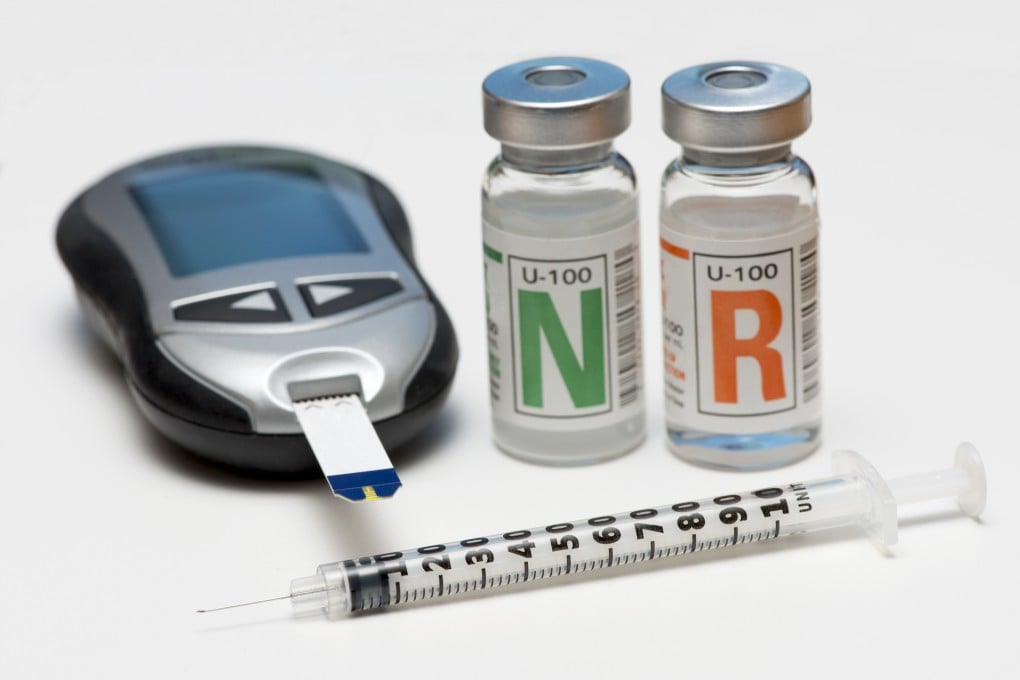
- Insulin technology has advanced significantly in the past century, from insulin pens and pumps to powder that is inhaled
This year’s World Diabetes Day on November 14 celebrates 100 years since insulin became widely available.
In 1923, type 1 diabetes changed from a terminal disease to a manageable chronic condition.
Since then, survival time after diagnosis has been extended from weeks or months to decades. Type 2 diabetes has become more easily manageable, even reversible.
Advances have made diabetics’ lives easier, but diabetes is still the ninth leading cause of death globally, according to the World Health Organization, and affects hundreds of millions of people (537 million in 2021). Type 2 diabetics make up 90 to 95 per cent of all cases.
How insulin saves my life
I was diagnosed with type 1 diabetes in 1996, aged 29, and saw the profound difference before and after my first insulin injections.
I am 6 feet 4 inches (193 centimetres) tall and in the few weeks before my diagnosis my weight dropped from around 90 kilograms (198 pounds) to less than 60kg.