Jack Ma Foundation backs Taiwan-born American scientist to develop a drug or vaccine to halt the spread
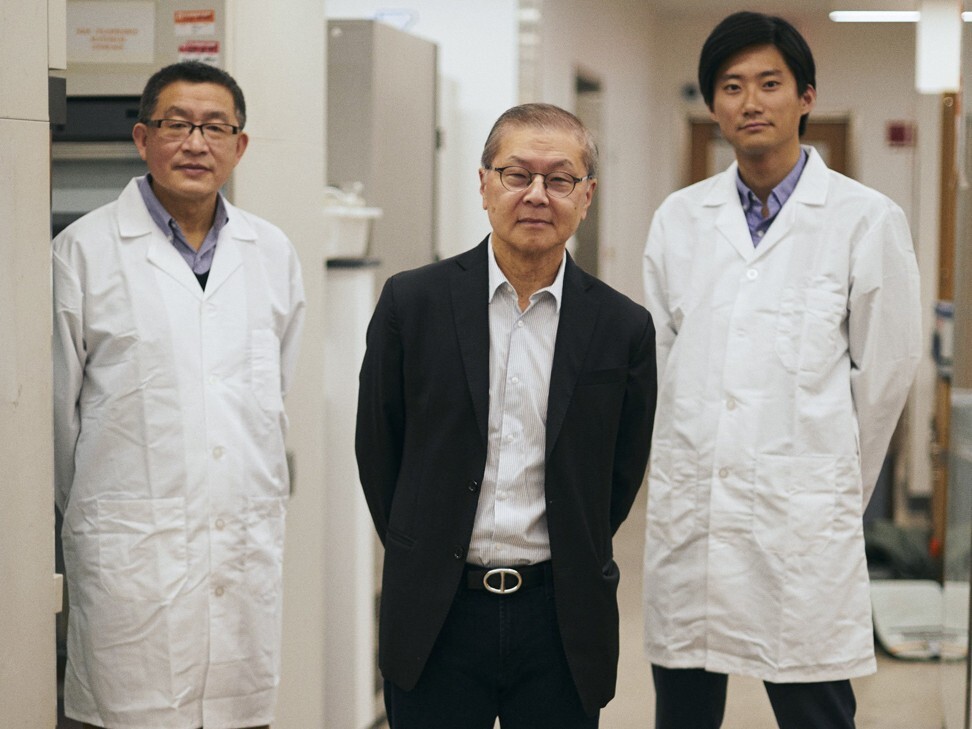
It seems obvious now that David Ho, arguably the world’s most famous Aids researcher, would get involved in seeking a treatment for Covid-19, the disease caused by the new coronavirus. It seems obvious the Taiwanese-American would redirect the work of his several dozen scientists at the Aaron Diamond Aids Research Centre, in New York.
But in late December, when Ho was tracking reports of a few cases of unexplained pneumonia in Wuhan, the capital of Hubei province, it wasn’t obvious he would be needed.
“We were paying attention but didn’t think we would get involved,” he says. “It seemed rare – and over there.”
In early January, as his lab changed its affiliation from Rockefeller University to Columbia University and moved to Upper Manhattan, the situation in Wuhan had become worse. Ho still wasn’t sure if he should get involved.
“The scientists in China were already doing so much,” he says. Many of those scientists – in Beijing, Hong Kong and Shanghai – are former students of his. “They could very well do the job.”
He had also seen funders lose interest in emerging diseases after the immediate panic about an outbreak subsided. Severe acute respiratory syndrome (Sars), for example, had been contained relatively quickly, in 2003, and as soon as it was, money for research became scarce.
Ho’s lab had developed antibodies that could have been used to pursue treatments for Sars, another coronavirus, but it was too late – he could not raise the US$20 million or so he needed to continue pressing forward on his own. “No one seemed to care,” he says. “That’s frustrating.” If he had found the money, it is possible he would be closer to a treatment for the new coronavirus.
Now, the virus has taken hold around the world. Counting the ill and calculating the rates of infection and death are daily, hourly exercises in caution and dread. The 1918 flu pandemic killed at least 50 million people. The HIV pandemic has so far infected 75 million and killed 32 million.
The death rate for Covid-19 appears to be much lower – it remains uncertain – but the illness spreads easily. If it reaches only 1 per cent of the global population, that would mean 75 million people would be infected, and at the current mortality rates, one million would die.
Scientists at Ho’s lab – and at Johnson & Johnson, Pfizer, Regeneron and at least 10 other drug and biotech companies – are working as quickly as they can to identify treatments. This virus is part of a family they have come to know. They are rushing to test old compounds even as they devise programmes to create new ones. Among the furthest along is Gilead Sciences, which is testing remdesivir – an antiviral drug developed to treat Ebola – on coronavirus patients around the world.
Scientists say they can tame this coronavirus, but for a while it will move faster than they will be able to. It may be a year or more before any specific treatment for Covid-19 is available. Until then we will have to contain it with distance and soap and the drugs we already have.
Even once there is a treatment, it is probable that Covid-19 will remain with us for longer than we would like. Completely wiping out something this widespread is exceedingly difficult, Ho is quick to say. Only one such virus has been eradicated: smallpox. That took about 20 years.
On an early March morning, before New York began closing down, Ho took some time to talk about the work under way at his lab. He wore a suit, and though he seemed perfectly comfortable, he would normally be in jeans. He would be busy, but his phone wouldn’t be constantly ringing. He wouldn’t be meeting with university trustees, or advising the NBA, or conferring with the head of China’s Centre for Disease Control and Prevention. He would be expecting his staff to have unpacked their moving boxes.
But this is not a normal time for anyone, and especially not for a scientist such as Ho. He was among the first to champion a powerful combination of drugs to attack HIV and to push for them to be administered early instead of after a patient developed symptoms. It was an unconventional approach that became the standard of care and helps explain why HIV is a chronic disease but not necessarily a deadly one.
It also explains why Ho was the first doctor to be named Time magazine’s Man of the Year, in 1996, and five years later was awarded the Presidential Citizens Medal. The plaque hangs on the wall behind his desk.

Ho is 67 years old, measured and focused, and central to a network of former colleagues and students who have known that a moment like this was coming: a pandemic that could be the biggest viral threat to humanity since HIV emerged in the 1980s.
Ho has developed an ambitious and expedited effort to come up with coronavirus drugs. The early stages of drug development typically take from five to 10 years, but he thinks it is possible to have the most promising compounds ready for animal testing in only one. His hope is to create a single pill that could treat this coronavirus and the ones that will come after.
“Surely there will be another one,” he says. “This is the third outbreak in two decades.”
“We’re reading strange literature about bat research,” Ho says. “Bats account for one-fifth of the mammals on this planet. That’s trivia we didn’t know. There are so many viruses that reside in bats – Sars and Ebola and perhaps this coronavirus.”

Covid-19 isn’t the first, and it won’t be the last. Ho wants to prepare for the next one now.
Hong had been an infectious disease expert at British pharmaceuticals giant GlaxoSmithKline and has known Ho for years. If Ho’s lab comes up with a drug, a big pharmaceutical company would have to come in to test and produce it. There is no formal agreement yet about how that would happen. There was no time for lawyers.
“Right now we’re just investing in faith and trust in the relationship and David’s reputation,” Hong says. “We just said, ‘Take the money.’”
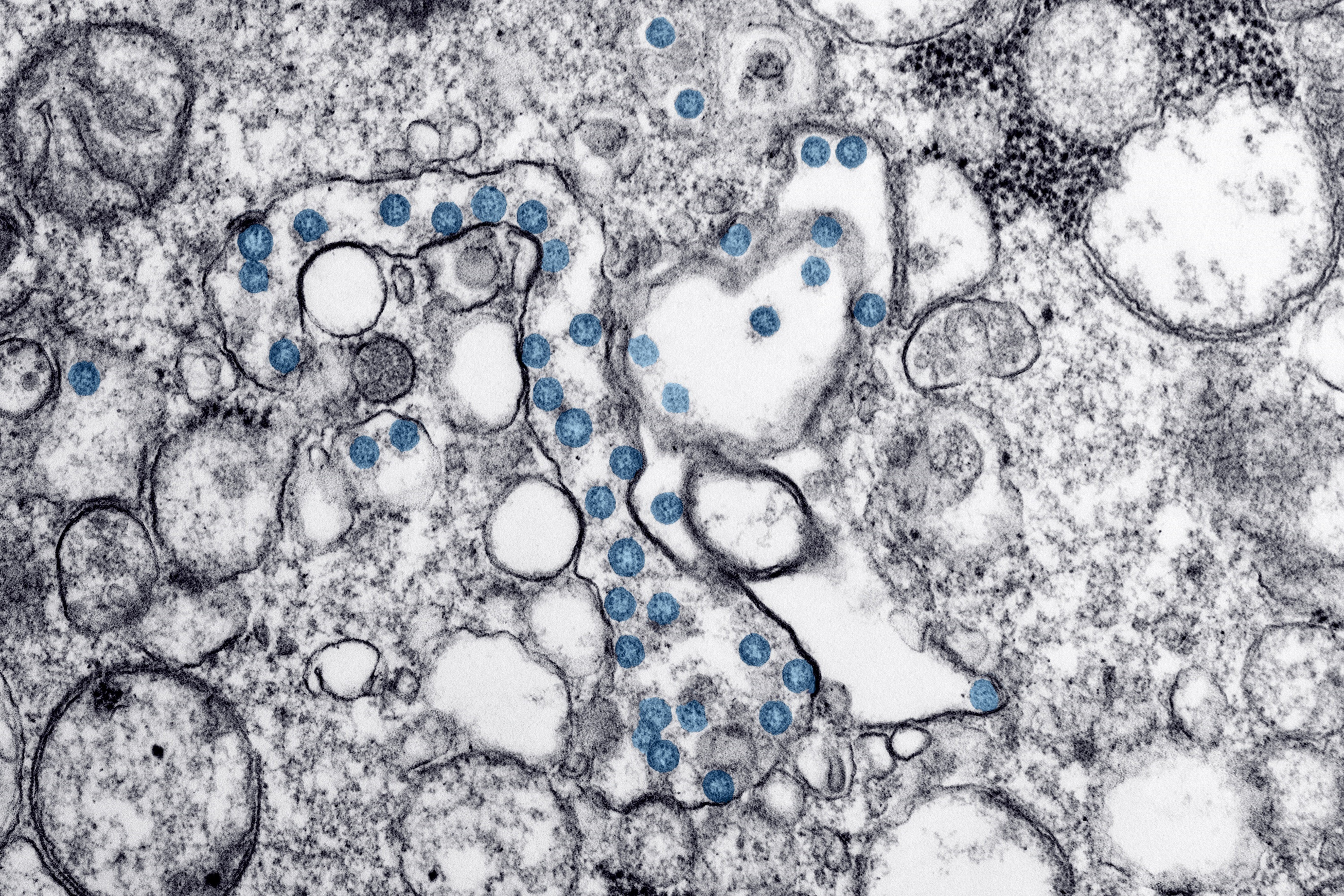
The most straightforward of the lab’s projects aims to find an antibody to block the virus from entering cells, either to prevent infection or to treat it. The first step was getting hold of specific white blood cells, called memory B cells, from patients who have recovered from Covid-19.
These cells, named because they can remember a virus for decades, contain markers on their surfaces that allow the body to rapidly generate many antibodies to that virus. These antibodies help protect against Covid-19 infection.

In late January, Ho called on his connections in Hong Kong to take blood samples from two convalescent patients. His New York staff spent days getting permission from the governments and arranging the shipping. The cells were purified, placed in tiny vials, frozen in liquid nitrogen at minus 150 degrees Celsius and sent to Ho’s lab by a specialised courier service. They arrived intact in late February.
As soon as they received the package, Ho’s lab went to work sorting out the B cells, extracting RNA, making DNA for numerous anti-coronavirus antibodies and expressing those antibodies on the surface of yeast cells. “Then we go fishing,” Ho says. “And we come with bait.” The bait is the spike proteins that protrude from the surface of the virus – or, in this instance, the lab-created pseudo virus. The tighter an antibody binds to the protein, the better.
“We pull out many, compare activity and select the best,” he says. “We could then change parts of the antibody to make it fit even tighter.”
The chances that this research, or similar research elsewhere, will yield a treatment are relatively high. The strategy worked for Ebola. Regeneron, which developed a successful Ebola antibody treatment, is also working on a coronavirus antibody “cocktail” and says human trials could begin by early summer.
But any such drug would have to be injected, which would likely require it to be refrigerated and administered by doctors – all of which would limit its use. It is not the ideal. But it might be good enough as a start.

Ho’s early HIV research focused on a crucial enzyme called protease, which acts as a kind of molecular scissors, cutting up viral proteins to help them replicate. One key set of drugs he tested on HIV patients in the 1990s were protease inhibitors: they interrupted that stage of the viral life cycle in an infected patient. He is hoping to identify potential coronavirus protease inhibitors, which would act in much the same way.
Alejandro Chavez, an assistant professor of pathology and biology at Columbia University, is helping Ho in this part of the research. Traditional labs at pharmaceutical companies test potential drug compounds on one viral strain at a time. Chavez has devised a radically different screening system that allows him to simultaneously test compounds on dozens – and if successful, find the ones that will work not only on Covid-19 but on other coronaviruses as well.
Chavez, 37, runs his own lab at Columbia, located across the street from Ho’s. In January, Chavez and Debbie Hong, one of the doctoral students working in his lab, were reading about the coronavirus like everyone else. When its genome was posted on a public-health website, they downloaded the sequence, found the protease gene and paid a bioscience company about US$80 to synthesise it.
Soon after, they got a call from Ho. “Ho nucleated a team,” Chavez says. Nucleated? “Yeah, he nucleated a team.” He means one of Hong’s thesis advisers at Columbia, Stephen Goff, decided to combine his research efforts with Ho’s. Then, because he knew Ho was still looking for university scientists to join his effort, Goff told him, “There’s these crazy people – maybe we should bring them in.”
That was Chavez, Hong and a few others in the lab. Ho was impressed by how rapidly they could screen the molecules that might inhibit all kinds of coronavirus protease enzymes; his search could be accelerated beyond what he could do on his own. “He wants to push it forward at warp speed,” Chavez says.

Chavez starts to explain his method. Then stops. Then starts. He has applied for a patent and is not sure how much he wants to reveal.
“I’ve never tried to explain this to a layperson and obfuscate at the same time,” he says. “I’ve only ever presented this once. I’ve been trying to stay stealth. OK, I’ll just disclose it.”
One of the problems with screening drugs against more than one viral protease at a time is that it is hard to tell which drugs are blocking which proteases. Chavez solved this problem by putting proteases from each virus into different cells, then creating what he calls name tags for each of the cells. He adds possible drug compounds to the cells and uses genome sequencing to read the tags, which allows him to see whether any of the viral proteases are blocked by each drug.
“I look at how abundant each of the name tags are – ‘How are you doing, Bob, John?’ – and I see if the protease is on or off. If it’s off, then that compound inhibited it. If the protease is on, then that compound didn’t do anything.”
Viruses aren’t just a threat, they’re essential to life on Earth
Chavez is speaking hypothetically. He is still working out the controls. “We’re not insane,” he says. “We’re going to be very methodical.”
Chavez was expecting to begin testing the actual compounds this month. In the meantime, Ho has been busy collecting those compounds from chemical libraries. He was able to obtain a curated selection of potential protease-inhibiting molecules from a research company in Shanghai called WuXi AppTec. The founder is a friend of Ho’s who received his doctorate in chemistry from Columbia. Chavez says that without Ho’s connections, his lab wouldn’t have known how to get such a high-quality collection of compounds so quickly.
It might take three to six months for Chavez to detect a few lead compounds that efficiently block coronavirus proteases. If – when – he does, Ho will connect him to chemists who will, over a matter of a few more months, increase the potency of the compounds by 100 per cent, maybe 1,000 per cent. “We know that kind of gain is doable,” Ho says.
It would be an important but still early step in creating a drug that would stop not only one viral protease but proteases from many coronaviruses. Because now we all know they are out there.
Text: Bloomberg Businessweek
